
In addition to the other "delights" of getting older, many people must look forward to a decline in knee function. A recent survey from Sweden found that self-reported knee complaints are influenced by age as well as gender. In their Knee Injury and Osteoarthritis Outcome Score (KOOS) study, the researchers found that women ages 55-74 voiced more knee-related complaints than men in the same group. On the other hand, older men ages 75-84 were more likely to report knee-related problems (BioMed Central Musculoskeletal Disorders, May 2, 2006, Vol. 7:38).
Naturally, imaging will play a major part in determining the source of all this griping about the knees. In a talk at the 2006 International Society for Magnetic Resonance in Medicine (ISMRM) in Seattle, Dr. Douglas Beall offered an update on MRI of the knee, discussing current topics and some old concepts with revisions.
Beall is the chief of radiology services at Clinical Radiology of Oklahoma and an associate professor of orthopedic surgery at the University of Oklahoma, both in Oklahoma City.
MCL tears
The traditional classification system for medial collateral ligament (MCL) injuries has been used to separate high-grade and low-grade injuries.
"This is one of the favorite classifications because it's grade 1, 2, 3. Grade 1 is a little bit torn, grade 2 is partial tear with disruption of the fibers, and grade 3 is completely torn," Beall said. "This is very useful because it has clinical applicability and (that) has to do with whether or not there's an end point (to the tear)."
 |
But this classification system tends to overestimate low-grade tears, Beall explained. The same fluid in or around the MCL that is generally a hallmark of low-grade tears can also be found with other entities, such as osteoarthritis, parameniscal cysts, and MCL bursitis. Beall suggested looking for other entities before attributing the fluid to an MCL injury.
Beall also cautioned that this traditional grading system tends to focus on the MCL when, in reality, this portion of the knee has a complex anatomic relationship with the posteromedial knee. MCL injuries may well involve other structures. In fact, isolated tears of the MCL are unusual, he said. Some of the most common are anterior cruciate ligament (ACL) tears, meniscocapsular separations, and osseous bruising.
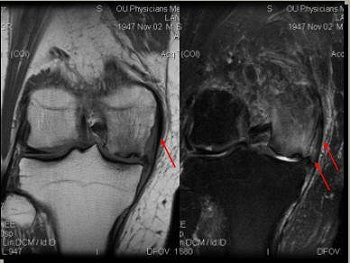 |
| Edema in MCL from osteochondritis dissecans (OCD) and chrondomalacia. |
Ligamentous lesions of the MCL may also be found in conjunction with displaceable tears of the medial meniscus. Beall cited a recent study that found a significant association between displaceable meniscal tears and with ipsilateral collateral ligamentous lesions, which generally resulted in greater pain as reported by patients (Radiology, January 2006, Vol. 238:1, pp. 221-231).
Identifying the location and extent of MCL tears, as well as injuries to related structures, can make a major difference for treatment options, Beall emphasized. For example, patients with a proximal disruption of the MCL may be candidates for conservative therapy, but only if it is partially torn.
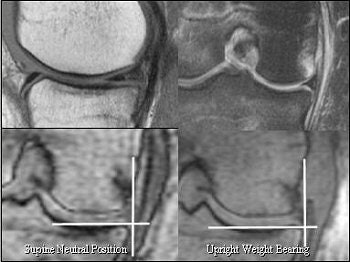 |
| Partially torn MCL with medial subluxation of medial meniscus. On the basis of MR measurements, no meniscal displacement was judged to be present in the supine 90° flexed position with external rotation or in the upright weight-bearing position. |
Also, tears of the posterior oblique ligament (POL) should not be confused with MCL tears. "Most people don't realize that the knee can be imagined in full extension. When the knee is unstable in extension, it's not an MCL tear. It's a tear of the POL," he said, adding that "whenever we talk about dynamic and static stability of the knee, the POL becomes very important because it can be fixed."
On MRI, the MCL is best visualized on axial or coronal T2-weighted images with fluid-sensitive sequences. The oblique coronal plane is optimal for evaluating the POL. These tears can be seen quite clearly on MRI and are usually not associated with a large joint effusion. "If you see a big knee joint effusion, look some more," Beall advised.
PCL injuries
The posterior cruciate ligament (PCL) tends to live in the shadow of the ACL, most likely because ACL injuries are more frequent and relatively easier to treat. PCL tears are typically under-recognized, Beall said, so a complete MRI evaluation is necessary.
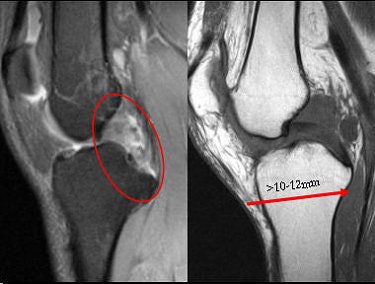
 |
Above, PCL tears that are likely to heal. Below, PCL tears that are not likely to heal.
 |
"The two basic injuries here are hyperextension and posterior force, which will disrupt the PCL. Historically, these are under-diagnosed, especially in athletes, because they have great quad strength, (and) great quadriceps muscle strength can make it difficult to examine these patients," he said.
In a recent study out of Italy, radiologists recommended T1-weighted spin-echo sequences integrated with T2-weighted and STIR sequences for a qualitative evaluation of PCL injuries. Massachusetts researchers found that proton density and T2-weighted sagittal, axial, coronal, and inversion recovery fat-suppression MR sequences were useful for detecting tibial eminence fractures and their relationship to other anatomic structures, including the distal PCL (La Radiologica Medica, August 11, 2006; Journal of Knee Surgery, July 2006, Vol. 19:3, pp. 187-190).
Beall pointed out that PCL reconstruction is an effective treatment method for an injured PCL, but controversy remains over repair versus conservative treatment. Unlike the ACL, even severe PCL injuries have been known to heal fairly quickly. But debate continues over a correlation between the location of the PCL injury and its propensity for healing. A PCL tear may be less likely to heal under the following conditions, Beall said:
- Complete tear of the anteriolateral and posteromedial bundles
- Associated MCL/posterolateral corner injury
- Post-translation greater than 10-12 mm on stress radiography
Presence of any of the above elements will most likely mean surgery, he added. "It really makes it necessary to have a complete MR evaluation so that if you have tears of both bundles that are really destroyed and (there's) not much left of the PCL, then we should think about (surgical) repair," he said.
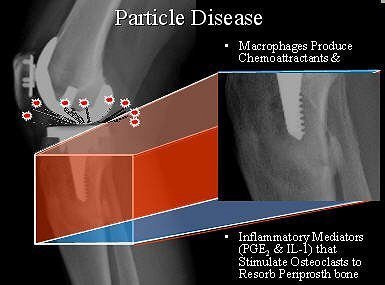
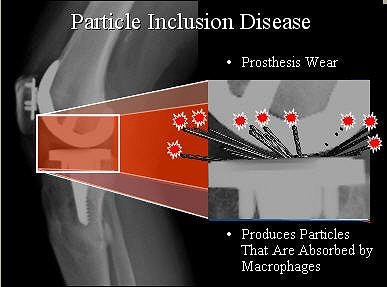
Particle disease
Particle disease results from wear of the prosthesis, causing loosening of joint arthroplasty and potentially affecting the longevity of total knee arthroplasty (TKA).
"The wear typically occurs medially and posteriorly, and this makes sense because the greatest biomechanical stress in the knee is about 28˚," Beall explained. "You get prostheses wear and this gives rise to particles. These particles are absorbed by macrophages. The macrophages then increase chemoattractants that bring in osteoclasts. Osteoclasts will be stimulated to resorb periprosthetic bone."
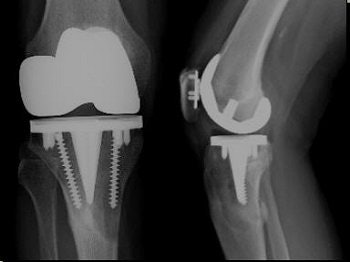 |
| Femoral components that may give rise to artifacts include cobalt chrome with polyethylene tip composition (most common), alumina ceramic, and Oxinium. |
The presence of metallic or ceramic components has limited the value of MR in assessing particle disease, but there ways around this issue, he said. First, he suggested that widening the receiver bandwith may decrease the size of artifacts, citing one study in which artifacts were reduced by 60% because a widened bandwith allowed for a broader range of frequencies to be sampled (Journal of Magnetic Resonance Imaging, September 2004, Vol. 21:7, pp. 745-753).
 |
Other technical tips that can make MRI of prostheses components feasible include increasing the number of excitations to compensate for the loss of signal-to-noise ratio, and increasing the number of refocusing pulses, which decreases the time for intravoxel dephasing. Also, widening the slice-select bandwidth may decrease misregistration between slices. Finally, view angle tilting (VAT) can be used to reduce metal artifacts, Beall said.
Final report
In summary, Beall stressed that the grading system for MCL injuries does have its value, but imaging experts should go one step beyond.
"What may be more beneficial is to describe the associated injuries of the MCL," he said. "It will give the clinician a better idea of what the clinical correlates of the anatomic MR imaging exam are and how to manage them."
As for the PCL, "PCL (injuries) will heal even if they are complete," Beall said. "Which tears don't heal? The ones with medial or lateral complex injuries, and tears that are associated with 10-12 mm or more posterior drawer."
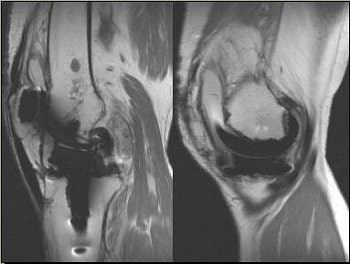 |
Above, 68-year-old female who underwent TKA in 2001. Extensive particle disease, suspected split through the polyethylene at the posteromedial margin of the tibial tray and diffuse resorption of bone around the femoral component, indicative of loosening. Middle and below, TKA with large burden of particle disease (red arrow), which caused loosening of the patellar backing (white arrows). All images courtesy of Dr. Douglas Beall.
 |
While the use of MR for particle disease is controversial, Beall pointed out that the modality, when used correctly, can clear up any confusion on other imaging tests, such as bone scan and arthrography, as well as offer a clearer picture of highly suspicious areas after total knee arthroplasty.
By Shalmali Pal
AuntMinnie.com staff writer
September 5, 2006
Related Reading
Case of the Day: Man twisted knee and cannot bear weight , August 5, 2006
ACL injuries aggravated by damage to associated ligaments, June 30, 2006
Knee joint cartilage loss linked to bone marrow lesions, June 7, 2006
Copyright © 2006 AuntMinnie.com



















