TORONTO - A PET/CT scanner using high-definition image reconstruction offers improvements in image quality for cardiac studies, according to presentations by U.S. researchers this week at the SNM annual meeting.
First introduced at the 2007 SNM conference, high-definition PET (HD-PET, Siemens Healthcare, Malvern, PA) was designed to correct for distortions caused by the circular geometry of commercial PET scanners, according to Ludovic Le Meunier, a Siemens employee based at Cedars-Sinai Medical Center in Los Angeles, where the system is being used.
The high-definition technique involves the use of a point source of radiation that's mounted on a 3D robot to measure point-spread functions across the field-of-view of an image to correct for distortions. Dedicated software is then used to reconstruct images, resulting in improved signal-to-noise ratios and uniform spatial resolution of 2 mm, compared to spatial resolution of 4.5 to 5 mm for filtered back projection (FBP) reconstruction and about 5 mm for ordered subset expectation maximization (OSEM) algorithms, Le Meunier said in a presentation on Sunday.
Although high-definition PET was originally targeted at oncology imaging, Le Meunier and Cedars-Sinai researchers decided to test the technique in cardiac imaging. They used high-definition PET in two groups of patients: 15 patients referred for resting cardiac perfusion assessment with rubidium-82 and 14 patients referred for myocardial viability assessment with fluorine-18 FDG.
Scans were performed on a Biograph 64 TruePoint PET/CT system (Siemens Healthcare), and images reconstructed with HD-PET were compared to three other reconstruction techniques: FBP, 2D attenuation-weighted OSEM (AWOSEM), and 3D AWOSEM. Cedars-Sinai's QPET software was used to analyze images for automatic detection of the left ventricle and reorientation of the heart and quantitative analysis.
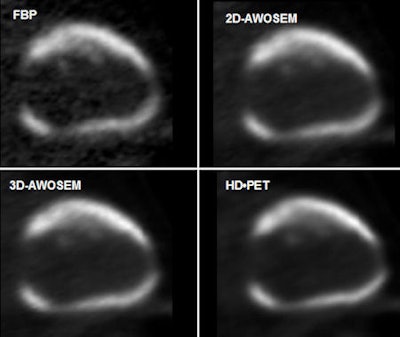 |
| High-definition PET produces better quality PET images compared to three other image reconstruction techniques, thanks in part to better contrast-to-noise ratios, according to Ludovic Le Meunier. Image courtesy of the author. |
The group found high-definition PET to be superior to the other reconstruction techniques in both the perfusion and viability patient groups. For the perfusion patients who received rubidium, the researchers saw contrast-to-noise ratio improvements as shown in the table below for static and gated patients:
Contrast-to-noise ratios, static versus gated perfusion patients
|
||||||||||||||||||
Improvement was also seen in the viability patients who received FDG:
| Contrast-to-noise ratios, static versus gated viability patients
|
||||||||||||||||||
The group also saw declines in the average wall thickness and myocardial volume on high-definition PET studies, but these differences were not statistically significant. High-definition PET was equivalent to the other techniques for ejection fraction, wall motion, and wall thickening, Le Meunier said.
In a Tuesday presentation, Le Meunier discussed the use of high-definition PET with an application of the QPET software designed to compensate for motion in the beating heart. In a study of 10 patients, the researchers saw improvements in contrast-to-noise ratio with motion-frozen high-definition PET: 4.5 for standard reconstruction, 5.3 for HD-PET, and 7.4 for motion-frozen HD-PET. Motion-frozen HD-PET images also demonstrated narrower wall thickness and improved the detection of heart defects, he said.
By Brian Casey
AuntMinnie.com staff writer
June 17, 2009
Related Reading
Cedars-Sinai explores PET's future in nuclear cardiology, April 11, 2008
Rubidium PET/CT shows potential for coronary artery disease diagnosis, March 30, 2007
Copyright © 2009 AuntMinnie.com



















