A new power combo consisting of adenosine stress and dual-energy CT (DECT) is delivering diagnostic accuracy equivalent to stress/rest cardiac MRI and nuclear perfusion (SPECT) for detecting perfusion defects, according to research presented at the American Heart Association (AHA) meeting in New Orleans.
DECT showed excellent agreement with MRI for delayed enhancement and performance equal to or better than SPECT for the detection of reversible myocardial ischemia, researchers from the Medical University of South Carolina (MUSC) at Charleston reported.
The addition of a pharmacologic stress agent in the study is a key step in the validation of DECT as a one-stop exam for examining the coronary arteries and diagnosing myocardial ischemia, said principal investigator Dr. Balázs Ruzsics, Ph.D., a fellow in cardiac imaging research at MUSC.
Along with the pharmacologic stress agent, the use of MRI to validate the DECT and SPECT findings was another important addition to the research protocol. Stress/rest MRI is a useful modality for the diagnosis of myocardial ischemia, as it provides sharp visualization of the relevant anatomy and enables physicians to distinguish reversible myocardial ischemia from permanently scarred or infarcted myocardial tissue. In this study, the results of DECT were closely correlated to those of stress/rest MRI.
"The new thing [with DECT] is really the status of the myocardial blood supply," said Dr. U. Joseph Schoepf, associate professor of radiology and medicine at MUSC, who joined Ruzsics in an interview with AuntMinnie.com.
"You can map the distribution of iodine in human tissues, and we've done that before under rest conditions," Schoepf said. With DECT "you create an iodine map and superimpose on it a grayscale reconstruction of the heart muscle. You see where the iodine is, and where there is iodine there is blood. Where the blood doesn't go there is a perfusion defect, and that's what we try and tease out with the dual-energy technique."
When the heart is burdened by a critical stenosis of the coronary arteries, the body releases waves of cytokines, which serve to keep the vessel maximally dilated. When adenosine is injected, it maximally dilates all of the vessels in a similar fashion, including the healthy ones.
With adenosine "you create a kind of steal effect ... and all of the sudden a certain portion of the heart muscle that is being perfused by the diseased vessel doesn't receive enough blood, and you can detect that as a perfusion defect with all of the perfusion imaging techniques," Schoepf explained.
Once the adenosine injection is stopped and the heart returns to resting status, another set of images is acquired several minutes later. At this point reversible ischemia can be distinguished from myocardial infarct.
"If you have a portion of the myocardium that was hypoperfused [during adenosine stress] but fills in during the rest scanning, this area is not really infarcted ... and that's what we call reversible ischemia," i.e., a perfusion defect that occurs during exercise but is not severe enough to cause an infarct yet, Schoepf said.
Added Ruzsics: "There is also a different entity, the so-called hibernating or stunned myocardium, that also has a reduced myocardial perfusion but the cells are still living. These are partially reversible defects, but we cannot see any [enhancement] in the delayed-enhancement scan. So whenever we see contrast in the delayed-enhancement scan regardless of whether it's CT or MRI, it means that the myocardium is infarcted and it's dead."
For this ongoing study, the researchers have examined 18 patients to date with known or suspected coronary artery disease, completing the data analysis for the first 15 patients. Of these 15 patients, 10 were male (average age, 60 ± 10 years) with an average body weight of 87 ± 19 kg. Nine of 15 had known coronary artery disease; six were at intermediate risk and three were at high risk for coronary artery disease based on Framingham Risk Score assessments. The average resting heart rate was 66 ± 9 beats per minute.
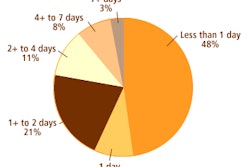
Within a week's time, each patient in the study underwent all three exams: adenosine stress/rest SPECT myocardial perfusion, adenosine stress/rest perfusion and delayed-enhancement cardiac MRI (1.5-tesla Avanto, Siemens Healthcare, Malvern PA), and ECG-gated adenosine stress/rest and delayed-enhancement DECT (Somatom Definition, Siemens), in dual-energy mode.
DECT
The team acquired three sets of CT images for each patient: at rest, during peak adenosine stress (140 µg/min/kg), and after a six-minute delay. The rest CT scan used retrospective ECG gating, 330-msec gantry rotation, 0.2 pitch, and 32 x 2 x 0.6-mm collimation, whereas the stress and delayed-enhancement scans were performed with thicker collimation and prospective ECG triggering, respectively, Ruzsics reported.
One tube of the dual-source system was operated at 181 mAs per rotation and 100 kV, and the second tube was set at 90 mAs per rotation and 140 kV. Rest and stress DECT scans were acquired following administration of two doses of 70 mL iopromide (Ultravist 370 mg iodine/mL, Bayer Schering Pharma, Berlin) using automated bolus triggering.
Similar to the other modalities, DECT scans began with an infusion of adenosine, during which time contrast injection also was initiated, Schoepf said. Low-dose thick-section CT angiography (CTA) images are acquired during stress to determine the presence of perfusion defects under stress, Schoepf explained.
When the adenosine stops and the heart rate returns to baseline, a second dose of contrast is injected and the patient is rescanned with a thin-section high-resolution coronary CTA.
The thin-section data are used to examine the coronary arteries and to see if the myocardial regions that were hypoperfused at stress fill in at rest, representing reversible ischemia, Schoepf said. The last scan is a prospectively triggered low-dose protocol to look for delayed enhancement representing infarcted tissue.
Three different reconstructions were performed from the single dual-energy CT data using the heart perfusion blood volume application in the DECT toolkit. The first set of transverse grayscale images -- the ones used to assess coronary artery patency -- were also used to optimize spatial and contrast resolution by merging 70% of the 140 kV spectrum and 30% of the 100 kV spectrum. A second set of images was based only on the 140 kV x-ray spectrum and a third on the 100 kV x-ray spectrum alone.
They analyzed the myocardial blood pool by assessing the iodine within the myocardium based on the unique x-ray absorption characteristics of the element at different kV levels. From these data, the color-coded iodine maps were created and superimposed onto grayscale multiplanar reformats of the myocardium.
Two experienced readers analyzed the morphology and stenosis grade with the aid of software, reporting stenoses ≥ 50% as significant. Two additional experienced readers, blinded to the results of other imaging tests, examined the rest/stress DECT-based iodine maps for myocardial blood-pool defects. A third experienced reader stepped in as needed for consensus.
MRI
Standard perfusion MRI images were acquired using a single-shot T1-weighted saturation recovery (SR)-true-FISP sequence with a TI of 250 msec (adjusted to null viable myocardium) and a TR of two cardiac cycles following injection of gadolinium and the adenosine stress agent. Sixty images were acquired in a 1.5-minute dynamic perfusion scan.
"Then the same sequence is performed at rest and compared with the stress images to see any perfusion defects, then we wait 10-12 more minutes and see the [delayed] contrast enhancement," Ruzsics told AuntMinnie.com.
SPECT
DECT iodine maps were compared to rest/stress SPECT myocardial perfusion imaging following injection of 370 MBq tetrofosmin (technetium-99m) at rest and 1,110 MBq at peak adenosine stress.
A triple-head camera system (Vertex 60+, collimator VXGP, Philips Healthcare, Andover, MA) with attenuation correction was used for ECG-gated data acquisition. Short and long axis images were reconstructed and evaluated for fixed and reversible perfusion defects by two experienced readers
DECT diagnostically equivalent
All patients were successfully imaged with all three modalities without adverse events. In the first 15 patients, 170 myocardial segments were analyzed and 15 were abnormal at cardiac MRI. There were four myocardial ischemia cases, seven cases of reversible ischemia, and four control cases, Ruzsics said.
 |
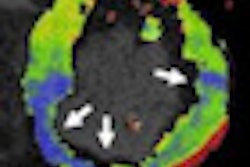
| Contrast-enhanced retrospectively ECG-gated DECT study in a 58-year-old man with abnormal SPECT. Short axis SPECT acquisitions during stress (A) and rest (B) show reversible perfusion defect in the left anterior descending (LAD) artery territory. Corresponding short axis DECT reconstructions reveal myocardial blood pool defects during both stress (C) and rest (D). DECT images show good agreement with perfusion cardiac MRI during stress (F) and rest (G) delineating a partially reversible subendocardial defect in the LAD territory. Late DECT image acquisition (six minutes after iodine administration) shows no sign of delayed enhancement (i.e., myocardial infarct; E). Similarly, there also is no evidence of hyperenhancement within the myocardium at delayed-enhancement cardiac MRI (15 minutes after gadolinium [Gd-DTPA] administration). All images courtesy of Dr. Balázs Ruzsics, Ph.D. |
Inter-reader agreement for detection of fixed or reversible perfusion defects and delayed enhancement at DECT was excellent (k = 0.9), the group reported. Compared with cardiac MRI, DECT and SPECT had sensitivity of 100% and 88%, specificity of 99% and 97%, and accuracy of 99% and 96%, respectively, for the detection of fixed perfusion defects.
Similarly, DECT and SPECT detected reversible ischemia with sensitivity of 100% and 100%, specificity of 100% and 90%, and accuracy of 100% and 92%, for the two modalities, respectively. And compared with cardiac MRI, DECT detected myocardial segments with delayed enhancement with sensitivity, specificity, and accuracy of 100%.
Among the 225 coronary artery segments evaluated in 15 patients, nine had significant (≥ 50%) coronary artery stenosis, including five in the right coronary artery, three in the left anterior descending territory, and two in the circumflex arteries. The study found one patient with three-vessel stenosis, one with two-vessel stenosis, and seven with single-vessel coronary artery disease based on coronary CTA, the authors wrote in an abstract.
 |
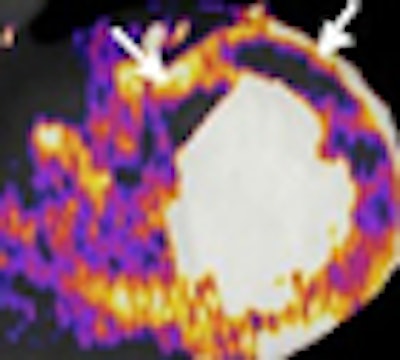
| Above, contrast-enhanced retrospectively ECG-gated DECT study in a 49-year-old woman with known coronary artery disease and previous history of unstable angina. Coronary CTA reconstruction displayed as curved multiplanar reformat (A) shows LAD stent with mild intimal hyperplasia (arrowhead) and noncalcified plaque with positive remodeling proximal to the stent (arrow). Short axis stress (B), short axis rest (C), and long axis rest (D) SPECT acquisitions show inferoapical fixed defect as a consequence of LAD infarct. Below, short axis DECT reconstructions show myocardial blood pool defect (arrows) in the corresponding inferior myocardial area during stress (E) and rest (F). Perfusion cardiac MRI similarly delineated inferoapical ischemia (arrows) during stress (I) and rest (J). Delayed-enhancement DECT in short (G) and long axis (H) views shows good agreement with delayed-enhancement cardiac MRI (K, L) for delineating nonviable, infarcted myocardium (arrows) represented by iodine accumulation at DECT and hyperenhancement at cardiac MRI. Long axis DECT (H) additionally reveals the presence of thrombus adjacent to nonviable myocardium. |
 |
Of 255 myocardial segments analyzed, 56 were abnormal at MRI. DECT showed excellent interobserver agreement (k = 0.9) for the detection of fixed or reversible perfusion defects, and delayed enhancement was excellent. Compared with MRI, DECT and SPECT had sensitivity of 100% and 88%, specificity of 99% and 97%, and accuracy of 99% and 96% for detecting perfusion defects. And compared to MRI, DECT detected myocardial segments with delayed enhancement with 100% sensitivity, specificity, and accuracy, Ruzsics and his colleagues reported.
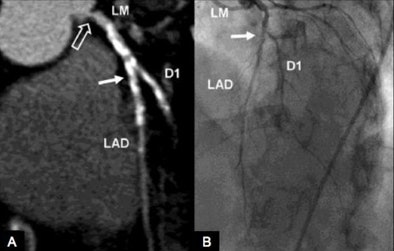 |
| Above, contrast-medium enhanced retrospectively ECG-gated coronary DECT angiography (A) and coronary catheterization (B) in a 75-year-old woman with atypical chest pain and suspected coronary artery disease. Anatomic coronary CTA reconstruction was performed using 70% of the high-energy and 30% of the low-energy x-ray spectrum of the rest scan and shows heavily calcified stenosis (solid arrows) of the proximal LAD and D1 branch in good correlation with invasive coronary catheterization, as well as ostial left main stenosis (open arrow) which could not be appreciated at coronary catheterization. The myocardial blood pool is analyzed by superimposing DECT-based iodine maps onto grayscale multiplanar reformats of the myocardium in short axis views, from which the iodine content in the voxels had been digitally subtracted using the Heart Perfusion Blood Volume application of the DECT reconstruction algorithm. Adenosine stress DECT (C) and stress perfusion cardiac MRI (D) at a mid-ventricular level both show ischemia (arrows) involving the anterior and anteroseptal left ventricle which is partially reversible at rest (E, F). Neither DECT after six minutes (G) nor delayed-enhancement cardiac MRI (H) show contrast media uptake in the ischemic territories compatible with stunned but not infarcted myocardium. |
 |
Pluses and minuses
"The workflow ... is basically the same for all three modalities and you get the same type of information as far as perfusion of the heart muscle, the one decisive difference being with CT you can evaluate the coronary arteries, which is of course something that you can't do with nuclear and you can't do with MRI," Schoepf said.
MRI does have the advantage of being a radiation-free exam, while the three DECT scans deliver a cumulative radiation dose of approximately 16 mSv for the average patient, he said.
Yet the CT dose remains lower than the typical sestamibi-based SPECT myocardial perfusion exam, which offers no anatomic information and cannot identify delayed enhancement. Other SPECT techniques, such as thallium scintigraphy, can identify regions of delayed enhancement, but at a cost of a radiation dose as high as 40 mSv, Schoepf said.
"The workup of a patient with coronary artery disease is not a free lunch as far as radiation is concerned," but CT still clocks in lower than the typical workup, he said.
A patient who undergoes a nuclear medicine scan gets an initial radiation dose of 10-40 mSv. If the results are abnormal, the patient is typically sent to the cath lab for invasive coronary angiography, adding another 4-15 mSv and a risk of complications.
"Overall, if you put all these numbers together and look at the risk profile of the invasive workup, I think CT looks pretty darn good both from the radiation perspective and from the risk profile," he said. "But with CT being the new kid on the block, there's much more scrutiny as far as radiation is concerned than for the more traditional tests."
The results showed that stress perfusion DECT is technically feasible and essentially equivalent to MRI, Schoepf said. But that doesn't mean he advocates it for the primary evaluation of myocardial perfusion," he said.
"If you have a [case] where you don't care about the coronary arteries, you just want to know about myocardial perfusion and viability, then you should always use MR for the primary evaluation," Schoepf said. "CT should only be used if the coronary arteries are of interest, which is the case in most patients ... but not always. So if you really want to have that one-stop shop assessment of coronary artery anatomy, and status of the myocardial blood supply, then I would use CT."
Several other groups at the AHA meeting discussed studies of CT myocardial blood pool imaging, presenting results that approached those of the MUSC study, he said.
"The dual-energy makes us a little bit more sensitive, I think, so our numbers stick out a little bit because of the increased sensitivity that you get from the spectral imaging component," he said.
By Eric Barnes
AuntMinnie.com staff writer
November 21, 2008
Related Reading
Dual-energy VC makes tagged materials disappear, October 29, 2008
Dual-energy CT helps distinguish malignant lung nodules, October 8, 2008
Dual-source CT edges into cardiac SPECT turf, March 6, 2008
DSCT matches angiography for stenosis detection -- even in fast hearts, December 4, 2007
CTA predicts functional recovery of the myocardium, September 7, 2007
Copyright © 2008 AuntMinnie.com