FDG-PET is a highly specific imaging modality for excluding acute osteomyelitis in the diabetic foot and is a useful imaging complement to MRI.
That conclusion comes from a University of Pennsylvania study that also found that FDG-PET should be the preferred imaging modality over plain film radiography when MRI is not allowed because of contraindications.
Diabetic patients who do develop acute osteomyelitis can suffer from necropathy of the foot and the loss of automatic motor responses. Those afflictions, in turn, can lead to further infection, prolonged trauma, and other related damage, noted study co-author Dr. Asad Nawaz.
Clinical signs of osteomyelitis also can be difficult to detect, he added, because two-thirds of the patients with diabetic foot disease are not going to present with signs of infection, such as fever or chills. In addition, approximately half those patients will not present with an elevated white blood cell count, making the clinical diagnosis very difficult.
Preventing surgery
"If we can diagnose osteomyelitis, we can prevent further surgical interventions and, hopefully, amputations," Nawaz said in his presentation at the 2008 SNM meeting in New Orleans. "Likewise, making sure we get the correct diagnosis, rather than a false positive, prevents patients from going through unnecessary surgery and amputations."
The goal for healthcare practitioners is to have one imaging technique that is highly sensitive and highly specific to minimize the number of procedures that are performed on patients. If one imaging technique is not ideal, then "a combination of techniques that would be highly sensitive and highly specific would become the ideal case," he added.
Current options for diagnosing acute osteomyelitis have their limitations. Nawaz noted that traditional bone biopsy is invasive and expensive, and it can take a long time to receive results. "The problem also is if a patient does not have osteomyelitis, doing a bone biopsy has the potential to have osteomyelitis induced because of the nature of the procedure," he said.
Plain film radiography is often the first imaging choice for healthcare institutions because the technology is more readily available and inexpensive. The modality, however, does not offer great sensitivity or specificity. "One of the problems in looking at osteomyelitis at the plain film level is that a lot of the signs you are looking for take two to four weeks to present," Nawaz said.
Study criteria
The University of Pennsylvania primarily uses MRI to diagnose osteomyelitis. This study and past research have shown that MRI has a high sensitivity but lacks in specificity. "One of the reasons is because the bone marrow signs -- the decreased T1 signs and increased T2 signal intensities -- don't necessarily have to be present with osteomyelitis alone," Nawaz said. Patients with fractures and postsurgery patients, for example, all present with the same bone marrow signs, making MRI a poor specific procedure.
In 2003, UPenn researchers began their study, funded by the National Institutes of Health (NIH), by analyzing patients who had undergone x-ray, FDG-PET, and MR imaging for osteomyelitis. Two diagnostic radiologists and one nuclear medicine physician interpreted the results. The readers were blinded to the patients' clinical symptoms and the findings of their colleagues.
For patients who had surgical intervention, researchers used pathology specimens to confirm the results. For patients with no surgical specimens or pathology reports, the study used clinical follow-up to determine osteomyelitis.
A total of 101 patients were enrolled in the study. Of the 101 patients, 24 had a diagnosis of osteomyelitis either from pathology and clinical follow-up, 32 cases were confirmed through pathology, and the remaining cases were confirmed through clinical follow-up.
FDG-PET's performance
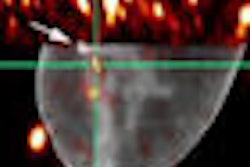
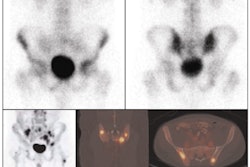
The researchers found that FDG-PET correctly identified acute osteomyelitis in 18 of 23 patients and correctly excluded acute osteomyelitis in 70 of 75 patients. Sensitivity was 78%, while specificity was 93%. FDG-PET's positive predictive value (PPV) was 78% and negative predictive value (NPV) was 93%.
MRI correctly identified acute osteomyelitis in 19 of 20 patients and correctly excluded acute osteomyelitis in 53 of 68 patients. MRI's sensitivity was 95%, while specificity was 78%. PPV was 56%, while NPV tallied 98%.
Plain film radiography correctly identified acute osteomyelitis in 12 of 21 patients and correctly excluded acute osteomyelitis in 52 of 61 patients. The modality's sensitivity was 57%, while specificity was 85%. PPV was near that of MRI at 57%, and plain film radiography's NPV was 85%.
MRI's NPV
Given MRI's high NPV of 98%, Nawaz said that if the modality does not detect osteomyelitis, "we can be fairly confident that it does not exist." The one concern with the study results with MRI is the low PPV of 56%, compared with 78% for FDG-PET.
"Although we can't say that any one of these techniques would be ideal in making the diagnosis of osteomyelitis," Nawaz said, "the fact that MRI does a very good job in excluding the disease and FDG-PET can be used to confirm the diagnosis of MRI was one of the results we got from our initial studies."
By Wayne Forrest
AuntMinnie.com staff writer
August 25, 2008
Related Reading
SNM's Images of the Year show molecular imaging's head-to-toe prowess, June 16, 2008
CMS declines PET coverage for infection, inflammation, March 20, 2008
SPECT/CT offers better bone scan views to enhance treatment, September 21, 2007
MRI keeps pace with rapidly evolving musculoskeletal systems of young athletes, May 20, 2007
Part II: Choosing between MR and US in musculoskeletal imaging, September 15, 2006
Copyright © 2008 AuntMinnie.com