Is virtual colonoscopy ready for routine clinical use? It depends on who's doing it and how, according to Dr. Andrik Aschoff. The mix of factors that make VC results so variable is one of the most complicated questions facing practitioners today, Aschoff said. But VC's popularity with patients is unmistakable.
In a "breakthrough applications" symposium at the recent 2005 European Congress of Radiology (ECR) in Vienna, he discussed the state of virtual colonoscopy today, and explored the often quirky relationship between radiologists, protocols, and results.
"We all know that the goal of CT colonography (VC) is to try to combine CT data with some kind of 2D and 3D postprocessing to obtain results similar to the ones that may be obtained with colonoscopy," said Aschoff, who is vice chairman of diagnostic radiology at the University of Ulm in Germany.
As they work to achieve parity with more invasive colonoscopy, relying on a myriad of techniques, VC researchers are finding their results all over the map. At one end of the scale is the outstanding 2003 study by Pickhardt and colleagues, who "developed a new gold standard by revealing the CT results to the endoscopists segment by segment after the colonoscopy," Aschoff said.
This group's results, achieved with a primary 3D reading technique in 1,200 asymptomatic patients, beat conventional colonoscopy, Aschoff noted. The team logged a sensitivity of 94% for detecting polyps 10 mm and larger, compared to 89% for conventional colonoscopy. The authors concluded that VC with 3D primary reading was accurate for detecting clinically relevant lesions, and compares favorably with optical colonoscopy.
"Sounds great, doesn't it? The question is whether it's really that simple for all of us," Aschoff said. "It sometimes reminds me of golf, which seems to be simple and easy for some, but very challenging for others."
Performance was clearly underpar for the Rockey trial, from the Duke University Medical Center in Durham, NC, which used methods not altogether different from those of Pickhardt et al, including segmental unblinding of the results, Aschoff noted. Yet there were also differences, including slightly wider 2.5-mm slices and 2D primary interpretation with 3D problem-solving, rather than the other way around. For polyps 10 mm and larger, sensitivity was a rocky 59%. On the other hand, the gastroenterologist-led trial logged 94% accuracy for conventional colonoscopy, Aschoff said.
"It's easy to believe the difference in colonoscopy (sensitivities), because criticism from gastroenterologists (of) the Pickhardt study was that they had really bad endoscopists in the U.S. -- and being at the European Congress of Radiology, we were ready to believe that," Aschoff quipped. "They also claimed that it was primarily surgeons doing the endoscopy, or whatever."
"Are we ready for clinical routine? In my perception it seems that Pickhardt is ready; Rockey is not ready," he said. "The question is are you ready?"
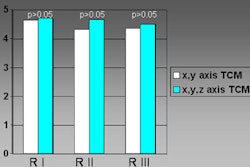
The problem with the question is that CTC and CTC are not the same thing, he said. One sees one group with 96% sensitivity, another with 58%, and any number of factors determining the difference, though the contributions of each factor aren't clear.
The Rockey population had positive fecal occult blood; Pickhardt's was asymptomatic. Pickhardt used a dedicated primary 3D interpretation method, while Rockey began with 2D. Then there is "CT protocol, postprocessing, experience of the reader, and we have to look at these factors to decide whether we are ready for routine clinical use or not," Aschoff said.
Whatever the exam, the rationale for colorectal cancer screening is compelling due to the well-known adenoma-carcinoma sequence, Aschoff said.
"If we have adenomatous polyps less than 1 cm in size, we have less than a 1% risk of these polyps becoming cancerous," he said. "But if you have 10 mm or more, you have a 10% risk of developing colon cancer over 10 years, and you have a 20% risk of developing cancer over 20 years. And if you find these polyps and remove them, you will not get cancer. This is why it's so important to screen for these polyps. And if you look at the population, we know we have many people who are 50 years old and older, and we have many polyps -- and we have to find them before they turn into cancer."
Accuracy inseparable from size
The efficacy of a VC technique always comes back to polyp size, and obviously it's easier to find the big ones than the small ones, Aschoff said. But the measure of a technique that should get the most weight is per-patient sensitivity, because finding one polyp that needs follow-up colonoscopy is what determines whether the patient gets an endoscopic examination. For this reason, per-patient sensitivities run higher than per-polyp sensitivities.
One clear trend is that sensitivities are improving as more detector rows are added to CT scanners, he said, showing a table published in 2002 that incorporated results from several VC studies. Most reported sensitivities for 5-8-mm polyps were below 50%, but they have been much higher in recent studies.
Many studies have also shown that collimation, pitch, and other factors wield an important effect on the detection rate of polyps, Aschoff said, referencing a 2002 report later published in Radiology in which a phantom was used to assess multiple variables of pitch, dose, and collimation, and measure their effects on polyp detection.
"Longitudinal distortion and rippling artifacts increased with increasing section thickness and use of broader detector collimation," wrote Dr. Johannes Wessling and colleagues from the University of Muenster in Germany in the study (Radiology, September 2003, Vol. 228, pp. 753-759).
"Polyps 8 mm or larger were depicted with any combination of section thickness, detector collimation, and tube current," the authors wrote. "Depiction of polyps 6 mm or smaller depended on the detector collimation/reconstructed section thickness, and was rated optimal for the 4 x 1.0-mm detector collimation with a section thickness of 1.25 mm. This was also observed for low-dose protocols. Polyps 6 mm or smaller that were not detected with 3-mm section thickness and 4 x 2.5-mm detector collimation were detected with 1.25-mm section thickness and 10 mAs."
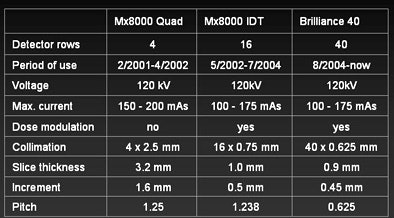 |
| VC protocol at the University of Ulm has evolved over the years with the installation of new MDCT scanners. Since 2001, slice collimation has shrunk from 3.2 mm to 0.9 mm. Chart courtesy of Dr. Andrik Aschoff. |
Measured against what
And although the sensitivity of virtual colonoscopy seems to vary widely, the optical colonoscopy gold standard it is measured against is unreliable, Aschoff said. When gastroenterologist Dr. David Rex and colleagues performed back-to-back conventional colonoscopies in 183 patients, they found that 24% of all findings were overlooked on one exam or the other, including 6% of lesions 10 mm and larger, he said (Gastroenterology, January 1997, Vol. 112:1, pp. 24-28).
Also note, said Aschoff, that the Pickhardt team found important lesions that conventional colonoscopy missed, including one of two colorectal cancers in a cohort that underwent both virtual and conventional colonoscopy.
But virtual colonoscopy has the same limitation of significant variability among readers, Aschoff said, citing a study by McFarland and colleagues that analyzed the results of four observers individually on multiple VC datasets. In the single-detector CT study, sensitivity for the detection of polyps 1 cm and larger ranged from 60% to 78% among the four observers.
(Pooled sensitivity was 0.68 for lesions 10 mm or larger [n = 40], with 75% agreement among the four readers, with greater variability for smaller polyp sizes, the authors reported in Radiology, November 2002, Vol. 225:2, pp. 380-390.)
Reaching more patients
So if endoscopy is good enough, why do we need virtual colonoscopy? The key is patient acceptance, Aschoff said. It's been said that patient preference studies published in gastroenterology journals often conclude that conventional colonoscopy is better, while those published in radiology journals find otherwise, Aschoff noted. As a result the findings are mixed. But in Aschoff's facility at the University of Ulm, both specialties are finding that VC has an edge.
The radiology department at Ulm has found that 27% of patients think VC is very comfortable, while 34% believe it's at least comfortable, Aschoff said. Meanwhile, the gastroenterologists at University Hospitals of Ulm report that 36% of patients consider conventional colonoscopy to be "very uncomfortable."
"So there's no doubt that CT colonography is preferred by some patients, and if you want to screen them, you have to get them into CTC," he said. (Aschoff said he dislikes the term virtual colonoscopy because it refers, technically, to 3D virtual endoscopy, which is only one of the CT techniques used to visualize colorectal lesions.)
The department is now equipped with a 40-slice CT scanner (Brilliance 40, Philips Medical Systems, Andover, MA) and Philips software (Virtual Colonoscopy Tool in EBW v2.0.1) that includes a "filet view" of the colon and well-integrated 2D backup, which is reliable and easy-to-use, Aschoff said.
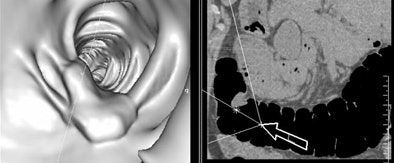 |
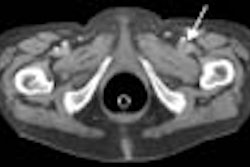
| Colorectal polyp seen in 3D endoluminal view (left) and 2D axial view (right). Images courtesy of Dr. Andrik Aschoff. |
For now the principal indication is failed conventional colonoscopy, "which happens fairly often," and an alternative to higher-risk endoscopy, he said. In the future, VC's widespread use for colorectal cancer screening is inevitable if it can be performed as well as Pickhardt's group has done it, he said.
By Eric Barnes
AuntMinnie.com staff writer
April 15, 2005
Related Reading
Senate hears testimony on virtual colonoscopy, March 28, 2005
Missed lesions offer lessons in VC, January 17, 2005
Multicenter VC trial begins with high hopes, state-of-the-art protocol, March 1, 2005
Duke VC trial results disappointing, November 1, 2004
Gastroenterology warning: Prepare for VC or regret it, October 6, 2004
Copyright © 2005 AuntMinnie.com