For the leading killer in the U.S., heart disease, coronary CT angiography's (CTA) ability to directly visualize the coronary arteries represents a huge medical advance capable of saving countless lives.
Indeed, a few short years after its introduction, coronary CTA has put several other common tests -- such as nuclear perfusion, stress echocardiography, and coronary calcium scoring -- on the path to obsolescence. But which patients benefit the most from coronary CTA? What about radiation dose? And why the massive organizational resistance to its widespread utilization?
Few are better equipped to address this subject than Dr. David Dowe, a radiologist and principal with Atlantic Medical Imaging in Galloway, NJ. Dowe, who scans thousands of patients annually with low-dose coronary CTA delivering 2 mSv or less of radiation, shared his experience, advice, and views of coronary CTA's place in the world at the 2007 RSNA meeting in Chicago.
"Now that dose has been conquered, coronary CTA should be without a doubt the first-line test for coronary artery disease," Dowe said. "We are already seeing the death of the negative diagnostic cardiac catheterization. My prediction ... is that five years from now the volume of stress testing will go down by 80%." Why? Because stress testing misses significant disease.
"Everybody knows the case of the guy who was worked up in the (emergency department), with negative troponin, negative (ECG), and dropped dead on the front lawn of the hospital," Dowe said. "We all have those cases and they happen every year. I'm a big fan of triple rule-out (coronary CTA) in a (prospectively) gated environment, which will come."
Besides, he said, CTA is an easy test and "not a workflow nightmare." You can learn to process 80% of your cases in five to 10 minutes or less, and it's only going to take you 100 cases to do that." But please don't try to learn CTA in a weekend, he added.
Two gating approaches
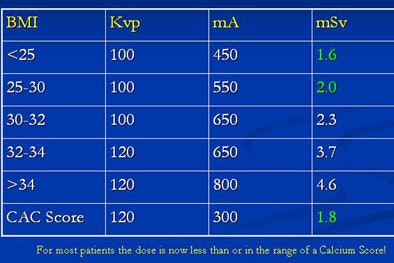
The difference between prospective and retrospective gating for coronary CTA is that the first irradiates the patient during a small portion of the cardiac cycle, while in traditional (and higher-dose) retrospective gating, the x-ray beam is on throughout the cardiac cycle, Dowe explained. The contrast injections are identical for both methods, and the settings are similar.
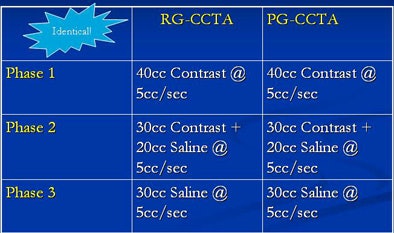 |
| Recommended contrast (above) and scanning techniques (below) are similar for prospective (PG-CCTA) and retrospective (RG-CCTA) gating methods. All images and data courtesy of Dr. David Dowe. |
 |
Retrospective gating allows the radiologist to go back at any time and reconstruct additional phases from the raw data, although three phases -- 70%, 75%, and 80% of the RR interval -- are usually sufficient when motion artifact is not a factor, he said. With retrospective gating, the dose can be reduced or modulated during phases far from systole that will not be needed for image reconstruction.
Dowe said he picks the maximum mAs from the body mass index (BMI) chart, and maximizes mAs at 40% to 80% of the RR cycle because once the heart rate is greater than 65 bpm, it's impossible to predict which phase will be needed to correct the segment with motion.
"I've fixed a ton of motion segments in the midcoronary (arteries) at 80% (RR) phase," and that's not supposed to happen, he said.
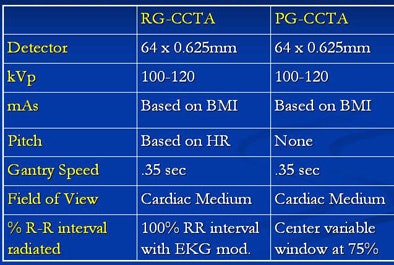
"Prospective gating is a different animal," Dowe said. "It's been used for years on calcium scoring. It's been around forever." The difference between prospective gating in the 80s and today is that today it's being performed on 64-slice scanners using 0.625-mm collimation.
With prospective gating the ECG machine takes control of the CT scanner, turning it on during a small portion of the cardiac cycle, and off the rest of the time, Dowe explained. Using a 64-slice scanner in step-and-shoot mode, the x-ray beam is on while it gathers 4 cm of image data, shuts off while the table advances, or "steps" to the next 4 cm, then acquires another 4 cm. The on/off switch is triggered by ECG R peak, with user-selectable time offset from the R peak. Up to 64 contiguous images are acquired for each gantry rotation within the same cardiac cycle depending on the scanner.
Therefore, the two-beat interscan delay in step-and-shoot acquisition mode is a gap in time, not space, and misses none of the vessel. And there's no need to pad the exposure window that is centered on 75% of the RR interval, Dowe said.
At a heart rate of 60 bpm, the RR interval is 1,000 msec in length. Using the rate-determined computer padding for step-and-shoot would irradiate 200 msec of that RR interval or 20% in addition to the 75% phase. However, this computer-selected padding can be overridden, radiating only 20 msec of the RR interval, or an additional 2%, in addition to the 75% phase, he explained.
"I never let the computer have that say," Dowe said. "Because ... if the heart rate is 65 or less ... I only need one phase. I don't need three phases. Some people will tell you to leave the padding ... it will help you get (rid) of motion. Nonsense! If the heart rate is less than 65, you're not going to have motion. Slam the pad down to 10 msec on either side of that 75% phase, and save the patient a ton of radiation."
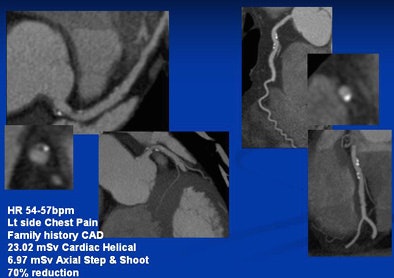 |
| Left main artery and right circumflex artery shows calcified and noncalcified plaque. The CTA dose was reduced from 23.02 mSv with retrospective gating to 6.97 mSv using prospective gating. |
Early cases revealed dose savings of 52% to 74% with the use of prospectively gated rather than retrospectively gated coronary CTA, Dowe said. Savings of 83% and more can be achieved in many patients with further adjustments in technique, such as dialing the kVp down to 100 from 120, which reduces the dose by an additional 38%. The images are indistinguishable.
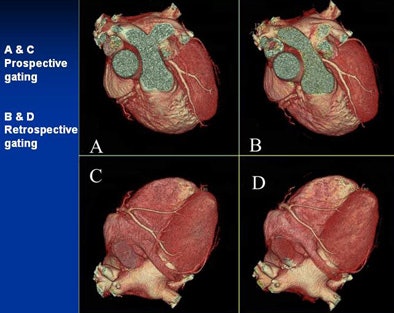 |
| Can you tell the difference between the low-dose prospectively gated and and higher-dose retrospectively gated coronary CTA images above and below? The acquisition method for each image is marked. |
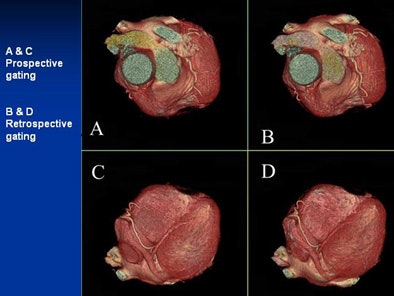 |
Keep in mind that reducing kVp to 100 increases image contrast, he said. Window and level settings should be routinely set at 1200/200 instead of the 800/100 used at 120 kVp. Like all prospectively gated coronary CTA, he said, the heart rate must be 65 bpm or less.
And if the patient's BMI range is on the border between two steps on the chart, be conservative and go with the slightly higher dose range, Dowe said.
 |
| Using prospective gating, Dowe and colleagues routinely obtain doses ranging from 1.6 mSv to 4.6 mSv, many in the range of a coronary artery calcium (CAC) scoring exam. |
"With a body mass index of 30 or less, you're going to get coronary CTA at or less than the radiation of a calcium score," he said. "This is the last nail in the coffin for calcium scoring, because you get the calcified plaque burden, the soft plaque burden, and the degree of stenosis in patients with BMIs of less than 30, which most of you are."
"I'm not. I'm up here at 30 to 32 (BMI)," Dowe said. "I'm one doughnut away from 32 to 34. But you know what? I had my coronary CTA a few weeks ago and my coronaries are pristine.... I'm having the doughnut."
As for limitations, most of the cardiac cycle is black with coronary CTA. And prospective gating can't be used for functional imaging. But a low-dose retrospectively gated exam can do functional imaging beautifully. And the prospectively gated triple rule-out is a "great test" at 12 mSv, he said.
Using a 64-slice LightSpeed VCT scanner (GE Healthcare, Chalfont St. Giles, U.K.) Dowe's center obtains prospectively gated doses ranging from less than 1 mSv for "Skinny Minnie" to around 8 mSv for the largest patients.
Radiation kills, Dowe said. For this reason beta-blockers should be used for every single coronary CTA exam.
"When someone tells me that on their scanner they don't have to use beta-blockers, I say, 'Fine -- I don't care,'" Dowe said. "Even if I had a scanner that had 10 tubes on it I would use beta-blockers, because the lower the heart rate on any scanner the less radiation. And radiation causes malignancies. There is going to be big-time pain to pay for the last seven years of this explosion in imaging," he said. "It's going to be leukemia and lymphoma in the years 2010 to 2020. Wait and see. Do we care about the dose? Absolutely."
Another dose-cutting tool are bismuth breast shields, he said. Use them on every woman who undergoes coronary CTA, and be sure to turn off the auto mAs feature so the scanner doesn't compensate, he said. The shields are inexpensive, they reduce the CTA dose by 40%, and they're comfortable for patients. "I'm wearing a pair now," he quipped.
The tone grew more serious as Dowe recounted the story of a business partner who had recently died. After a myocardial infarction in 1994, the patient had annual nuclear stress tests from 1995 to 2006, in addition to two coronary CTAs and a coronary angiography. In 2004, the patient had radiation therapy for prostate cancer. In 2006, he was diagnosed with acute myelogenous leukemia (AML), and died in 2007.
"I will go to my grave knowing that he died of radiation-induced malignancy," Dowe said. "Is that important to you? It had better be."
CTA as political football
On the other hand, CTA has been the perennial whipping boy when it comes to radiation dose, and unfairly so, according to Dowe.
"Nobody cared about radiation dose until coronary CTA came on the market and broke up the monopoly on coronary artery disease workup," he said. "It was a political football from day one." Anyone who thinks their test can compete with CTA need only look at prospective gating and "you're toast," he said.
In particular, the prospectively gated triple-rule out is a "great test" at 12 mSv, he said. This test renders turf battles moot. Even full-dose, retrospectively gated CTA was always in the range of SPECT studies, he said. "And who complains about number of SPECT studies being done? Before coronary CTA, there was no talk of dose, Dowe said.
"I've had plenty of tough meetings with hospital administrators, with cardiology wanting to do this, and radiology wanting to do that," he said. "Up goes the radiation dose and they say there's too much radiation from coronary CTA." When he responds by asking how much radiation comes from the SPECT studies being done, "the room gets pretty quiet," he said.
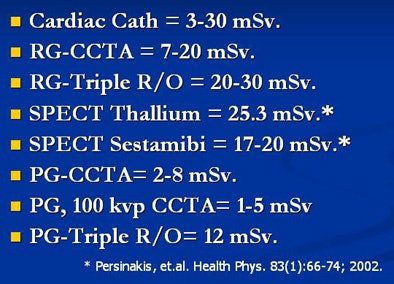 |
| Typical radiation dose from other diagnostic cardiac studies is high (PG = prospectively gated; RG = retrospectively gated). |
CTA should be the first-line test right now for ruling out coronary artery disease, Dowe said. "Why is it so different from CTA for pulmonary embolism (PE)? We went from a V/Q lung scan to CTA for PE. Where were the long-term, prospective, double-blind, randomized trials that said CTA was OK for PE? It was obvious to us that it was better. And I think it's obvious that coronary CTA is better than the stress test as a first-line exam."
Commenting last week on the recent push to limit Medicare reimbursement for payments for CT angiography, Dowe wrote in an e-mail to AuntMinnie.com that he believes only the health insurance industry could be interested in curtailing coronary CTA.
"I was part of a panel discussion representing the (Reston, VA-based American College of Radiology) at a national meeting of Blue Cross Blue Shield medical reps, and it was clear that they feel (coronary) CTA will be an add-on test and not replace other tests," Dowe wrote. "This is based on their history with imaging and specifically cardiac imaging. They don't buy into the fact that (coronary) CTA replaces many cardiac caths, which is documented in the literature. They also don't share in the opinion that (coronary) CTA will replace, in most instances, the nuclear stress test, which has a higher reimbursement and higher radiation dose."
Risk factor roulette
Unfortunately, a patient's risk factors don't tell you who has coronary artery disease; only direct visualization does, Dowe said. In the course of dozens of stories Dowe related in his RSNA presentation, some of the patients were found to have multiple risk factors, perhaps a long smoking history, family members who had died of heart attacks -- and completely clear arteries. Others exercised daily and ate their sprouts, and CTA revealed severe disease just in time to save them. Another patient had significant calcified plaque at age 27.
"You think you can predict coronary disease? You can't," Dowe said.
Certainly coronary CTA will overcall some disease, he said, because unlike coronary angiography, the images are rotated to the point where the stenosis is largest. But a false positive is not the end of the world like missing lethal coronary artery disease is. CTA excels in determining who doesn't have coronary artery disease. And it outperforms the stress test, which yields false positives of its own. Stress test false positives are the reason why 50% of catheter angiography exams are negative, Dowe said.
When is CTA indicated? Dowe said that, in general, he believes that many of the recommendations published in 2006 guidelines are too conservative (Journal of the American College of Cardiology, October 3, 2006, Vol. 48:7, pp. 1475-1497).
Take presurgical clearance. The guidelines say the utility of CTA is undetermined, but the literature has been very positive, Dowe said. You might overcall a stenosis but you won't overcall a cardiomegaly. What about asymptomatic patients with stents?
"I think the main question is, how old is it, will a negative CTA stop the workup, and what is the pretest probability of (coronary artery disease)?" he said. An asymptomatic patient with previous coronary artery bypass grafting is trickier, because grafts fail over time. A positive CTA result won't change the management, so stick to the stress test for this patient.
"With a stent it's a different story," Dowe said. The coast is clear with a negative CTA, "but a positive coronary CTA with a stent will give you a stress test nonetheless if the patient's baseline stress test is abnormal."
Conclusions
"This is a great moment in CTA's life cycle," he said. "We are uncovering a new class of patients: the stress test-negative, coronary CTA-positive patients. Eighty-five percent of myocardial infarctions (MIs) come from eccentric soft plaque that ruptures; only 15% of MIs come from stenosis. And the only thing that's going to see those soft plaques is coronary CTA."
CTA is superior for detecting 50% and greater stenosis, he said. The stress test isn't even in the game. CTA provides rapid, safe diagnosis with superior positive and negative predictive values compared to alternative tests in the setting of acute chest pain. CTA is excellent for preoperative clearance of the heart. It prevents unnecessary admissions and inappropriate discharges, Dowe said.
CTA detects serious extracardiac findings in about 1% of patients. "It gets the right people on statins and the wrong people off them," he said. It is cheaper, less time-consuming, and produces far less radiation than nuclear SPECT.
There are more than 1,000 64-slice scanners in the U.S., and the test is potentially available 24/7, though radiologists are loathe to admit it, he said. And CTA has major advantages in the rural setting.
"I think this thing is going to be colonoscopy of the heart," Dowe said. "You're going to get one at 40 if you're a man, 50 if you're a female. Why? Because you have a heart. Why get colonoscopy? Because you have a colon. Why does a woman get a mammogram? Because she has breasts. Why should we fool around with risk factors and Framingham scores and stress tests and calcium scores and ... carotid intimal media thickness? Why should we do all this -- dump all this information into a barrel and say the great swami says based on all this information I think the coronaries look like this -- when we can do a six-second scan with 90% less radiation than a stress test and just look at the darned arteries?"
By Eric Barnes
AuntMinnie.com staff writer
January 17, 2008
Related Reading
Coronary CTA study aims for lowest dose, January 11, 2008
Pending Medicare decision roils cardiac CTA, January 8, 2008
Low-dose coronary CTA diagnoses most patients, November 28, 2007
Radiation dose slashed in 64-slice coronary CTA, February 15, 2007
Step-and-shoot acquisition cuts CTA dose, improves images, January 16, 2006
Copyright © 2008 AuntMinnie.com