Take one part 3D echocardiography and one part SPECT, acquired during the same imaging session. Combine the two with an automated image fusion algorithm, and what do you get? A way to image patients with coronary artery disease (CAD) that improves upon the performance of 3D echo or SPECT alone.
That's according to a group of researchers who combined 3D echo and SPECT in a "feasible and promising" clinical setting and added newly developed image processing algorithms to enhance the detection of coronary artery disease.
"The combination of fused real-time 3D echocardiography and SPECT plus interactive, quantitative analysis has excellent potential for accurate detection of wall motion abnormalities and improved diagnosis of ischemia with underlying coronary artery disease," the authors wrote.
The research was published in the February issue of the Journal of Nuclear Medicine (February 2009, Vol. 50:2, pp. 226-230).
Researchers from Ohio State University (OSU) in Columbus, the Cleveland Clinic in Ohio, the University of Maryland in Baltimore, and Mount Sinai Hospital in New York City collaborated on the study. Lead author Vivek Walimbe, Ph.D., secured funding from the American Heart Association (AHA) as part of his fellowship research at the Cleveland Clinic and OSU from 2004 to 2006.
Previous research, Walimbe said, has shown that "3D echocardiography has good specificity in terms of determining coronary artery disease, but it is not very sensitive. So we started looking at what is the complementary modality for echocardiography that gives good structural information."
Complementary modality
SPECT, he added, is a natural complementary imaging modality to provide perfusion and blood flow information for the cardiac muscle. "In terms of the accuracy of the procedure, SPECT is very sensitive, but it gives you a lot of false positives," he said. "Still, there is a complementary synergy between the two modalities. They both give different types of information; they have different strengths and weaknesses."
By performing scans with the two modalities during the same patient session, the researchers sought to prove that the approach can offer a direct correlation between myocardial perfusion and anatomical images during diagnosis, eliminating "the confounding effects of suspected artifactual defects commonly encountered during diagnosis based on echocardiography and SPECT individually," the study noted.
The two-year study recruited 20 consecutive patients, ranging in age from 45 to 75 years; the average age was 62 years. There were 14 men and six women in the study with known or suspected CAD referred for stress SPECT.
Five patients had a known history of myocardial infarction, while seven patients had known coronary intervention or cardiovascular surgery. The researchers excluded patients with known atrial fibrillation
Image processing
Pre- and poststress SPECT image sequences consisted of eight frames each to cover the entire cardiac cycle. Images were acquired by a dual-head gamma camera (Siemens Healthcare, Malvern, PA). Left ventricular real-time 3D echocardiography images between 15 and 20 frames per cardiac cycle (twice the temporal resolution of SPECT), depending on patient heart rate, were acquired using an iE33 ultrasound scanner (Philips Healthcare, Andover, MA).
The researchers added the 3D echo scan to an already planned SPECT cardiac stress with technetium-99m sestamibi and rest procedure and acquired the 3D echo images at the peak of pharmacologic stress.
"As you reach the peak stress of the heart rate, that's when, in the clinical protocol, you would inject the [sestamibi (MIBI)] contrast agent to collect the perfusion information," Walimbe said. "The important thing is to do it at that time, because you want to lock in the perfusion when the heart is at peak stress. As soon as you inject that, you don't need to do SPECT imaging for the next 20 to 40 minutes to give [the patient] time to stabilize."
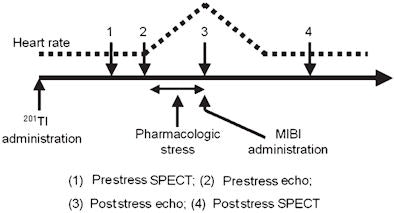 |
| Diagram shows the process of clinical image acquisition and corresponding variation of patient heart rate. The 3D echo image is acquired at peak (3) of poststress echo. 3D echo adds approximately five minutes to scan time. All images courtesy of the Journal of Nuclear Medicine and Vivek Walimbe et al. |
The addition of the 3D echo scan adds only five minutes to the exam time. "And with echo, there is no radiation," Walimbe added, "so you are not doing the patient any harm and checking a lot of useful information."
A nuclear cardiologist with expertise in reading both echocardiography and SPECT images reviewed all 20 cases, using the interactive and quantitative multimodality image-analysis software.
During the clinical stress protocol, all study participants reached or exceeded the 85% maximum predicted heart rate considered necessary for inducing diagnosable myocardial ischemia in the setting of mild-to-significant CAD. Simultaneous pre- and poststress real-time 3D echocardiography and SPECT and all fully automatic preprocessing steps were performed successfully in all 20 patients.
Diagnoses of real-time 3D echo, SPECT, and fused imaging in 36 coronary arteries
|
||||||||||||||||||||||||||||
| Source: the Journal of Nuclear Medicine and the Cleveland Clinic. | ||||||||||||||||||||||||||||
Once the images were acquired, they were fused using internally developed software that both registers the different images and provides a means of quantitatively reviewing and analyzing the results. Readers using the software were able to assign diagnostic ratings for all 17 segments for each case.
The researchers' recently created algorithms are the key components to the success of the dual-modality scan.
"There are a lot of technical challenges, in terms of getting these images, because they are different native spatial resolution and temporal resolution, in terms of the many frames required to cover the heart cycle," Walimbe said. "The second part is doing the automated quantitative analysis. You can provide the physician with additional help in terms of evaluating wall motion, wall thickness, and perfusion information, and putting the images together along with this quantitative information. That enhances the diagnostic capabilities."
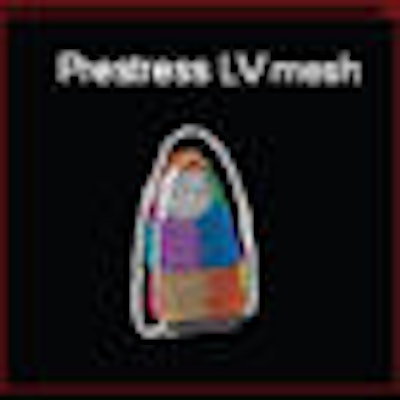
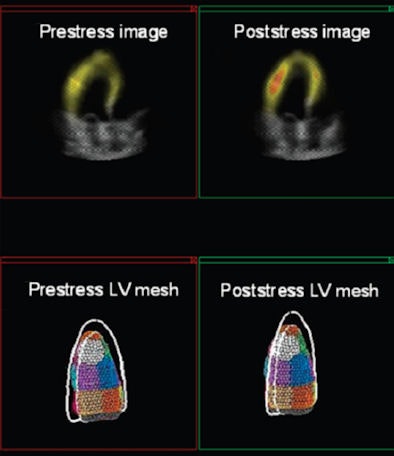 |
| Matching pre- and poststress fused images (top, 3D echo and SPECT) are available after alignment of images using registration techniques. Corresponding left ventricle meshes (bottom) are obtained using automatic segmentation technique. |
The hybrid scan approach is not in regular clinical practice yet. Walimbe said a much larger clinical trial is needed with more patients across different age groups to verify the efficacy. "One of the limitations of our study is that we only had 20 patients," he added. "To bring it into clinical use, the next step would be to prove it in a much larger study."
That extended research is the focus of Dr. Raj Shekhar, one of Walimbe's collaborators, at the University of Maryland School of Medicine.
By Wayne Forrest
AuntMinnie.com staff writer
February 12, 2009
Related Reading
Nuclear myocardial perfusion imaging: Vulnerable to self-referral? December 15, 2008
SPECT MPI predicts sudden cardiac death, September 26, 2008
Echocardiography method predicts CAD, September 16, 2008
Quantitative stress echo can reliably find coronary artery disease, August 18, 2008
PET, SPECT measures of LVEF have superior predictive value, March 13, 2006
Copyright © 2009 AuntMinnie.com