BOSTON - Across most of the U.S., virtual colonoscopy practice is a low-volume affair, relegated by lack of reimbursement to a few diagnostic indications and follow-up after incomplete colonoscopies.
Then there's Wisconsin, where Dr. Perry Pickhardt and his colleagues at the University of Wisconsin Hospital and Clinics in Madison have built a bustling VC practice based primarily on reimbursed screening exams for mostly asymptomatic subjects 50 and older.
"This is a very exciting time for VC as we move from validation for screening to actual implementation and patient care," Pickhardt said on Tuesday at the International Symposium on Virtual Colonoscopy.
In a discussion of population-based screening VC in the U.S., Pickhardt said he is optimistic that given recent improvements in technology and study results, insurers in the rest of the country will reimburse VC for screening within the next year or two, a time line that beats other educated guesses by at least a couple of years.
That said, VC is still working through performance issues that are being addressed, turf issues that may be overstated in current discussions, and the National CT Colonography Trial (ACRIN 6664) results expected next year, which will also impact VC's near-term prospects.
Insure this
Beyond that, payment is in the hands of payors, and it often takes something of a critical mass to move them in the direction of screening coverage, said Pickhardt, who is an associate professor of radiology at the University of Wisconsin in Madison. Today the safe route for most health insurers is to simply hold off and wait for others to dive in first, he said.
"Most payors are tied to some kind of national plan, and they can easily just point to the national view that CTC (CT colonography or virtual colonoscopy, VC) is just investigational," he said.
Others may be focused on short-term financial results, while netting the anticipated downstream financial benefits of a colorectal cancer screening program takes many years.
"If a third-party payor decides overnight to cover screening VC, they're going to take quite a hit in the short term, opening up the floodgates if you will," Pickhardt said.
So although comprehensive colorectal cancer screening may be a long-term winner, the screening money has to be spent now, he said. And some healthcare executives aren't in a position to take the long-term view, he added.
"I know that real-life implications affect some of these decision-making processes," Pickhardt said. "I know our local payors that now cover screening, at least two of them wouldn't have agreed to do it unless somebody else had said yes."
Just this month, someone else said "yes." Pickhardt announced during his talk that Wisconsin Physician Services, a statewide healthcare organization based in Madison, has agreed to extend screening VC coverage to all of its covered members in Wisconsin upon preauthorization, though the new program could not be verified with the insurer by press time.
For now, only the University of Wisconsin Hospital in Madison will provide the exams, but other so-called centers of excellence are envisioned for other parts of the state, Pickhardt said.
A screening practice
The center screens from 200 to 250 mostly asymptomatic patients with VC per month, about 3,500 in all since reimbursed screening began in 2004 on the heels of a successful multicenter VC trial by the U.S. Department of Defense (DOD) and on the good will of a few local payors in Wisconsin (New England Journal of Medicine, December 4, 2003, Vol. 349:23, pp. 2191-2200).
C-RADS reporting criteria have been used from the start, Pickhardt said. That is, screening patients with detected lesions 10 mm and larger are referred for colonoscopy, and those with one to two polyps 6-9 mm in diameter are offered colonoscopy or alternatively a surveillance program, which about two-thirds opt for (Radiology, July 2005, Vol. 236:1, pp. 3-9).
Patients referred for colonoscopy have their studies the first day, which wouldn't be possible without a cathartic bowel preparation regimen.
"This is the real strength of a cathartic (prep) VC study, in addition to being probably the most accurate approach. Avoiding a second prep is a huge issue that I think we're going to have to tackle if we go to a noncathartic exam," Pickhardt said.
In the prepless VC scenario, a patient who undergoes a VC exam yielding suspicious results will have to begin a cathartic bowel prep the next day, returning on day three for conventional colonoscopy. Should conventional colonoscopy then show that the VC finding was a false positive, there would likely be negative repercussions, Pickhardt said.
At the university facility, results have improved significantly and consistently since the days of the DOD trial, mainly due to technical improvements in the exam, he said.
"Why are we doing better? I think it's multifactorial," Pickhardt said. "These are all new radiologists, and I'm the only one that crossed over (from the DOD trial). So it isn't really about experience."
There are five radiologists on the team. Significant among the technical factors that have improved the exam is better colonic distension, resulting from the use of automated CO2 insufflation (ProtoCO2l, E-Z-EM, Lake Success, NY) rather than room air, Pickhardt said.
In addition the workstation software (V3D Colon, Viatronix, Stony Brook, NY) has also evolved since the trial, he said, and fly-throughs are now twice as fast and just as accurate. Improvements in cathartic cleansing technique are delivering better datasets. Finally, four- and eight-slice scanners have been replaced with 16- and 64-slice models (GE Healthcare, Chalfont St. Giles, U.K.), although Pickhardt said he believes 64-slice scanning isn't really necessary for virtual colonoscopy.
Pickhardt believes that it is these improvements that have produced significantly higher positive predictive since the DOD trial (less than 60%) to approximately 90% today, with substantial positive impacts on the cost and efficacy of the exam.
Just-published results from the first year of the screening program, for example, show that among patients who went on to polypectomy after VC, more than 90% of the time the gastroenterologists found the same lesions patients were referred for, Pickhardt said.
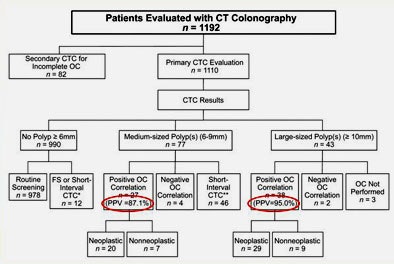 |
| Results from 1,192 patients screened with VC and referred for optical colonoscopy during the first year of the program show a high correlation between VC and OC results, yielding a positive predictive value of 87.1% for medium-sized polyps and 95% for polyps 10 mm and larger. All images and data courtesy of Dr. Perry Pickhardt. |
In addition, the implementation of large-scale VC has not reduced the volume of colonoscopies; with more patients being screened, volumes have improved for both exams.
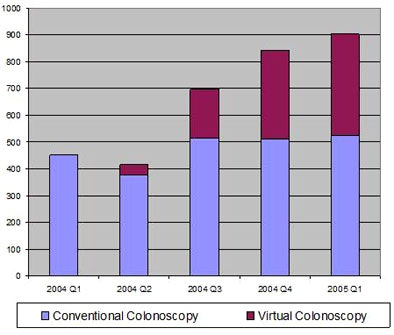 |
| Since the VC screening program began in the first quarter of 2004 at University of Wisconsin Hospitals, referrals to optical colonoscopy have risen. Patients have a choice of VC or colonoscopy for first-line screening. |
"This flies in the face of models that say VC is going to impact (gastroenterologists') exam volumes," he said. "As this whole VC thing takes off ... I think it will improve (gastroenterology) practices in many ways" -- for example, by ensuring a higher percentage of therapeutic colonoscopy exams, he said.
At the same time, results from the first 3,000 of the 3,500 patients show that VC has done a pretty good job of getting people off of the colonoscopy treadmill, Pickhardt said. In the fairly healthy, typically 50-something population that undergoes screening in Wisconsin, about 80% have no medically significant polyps, another 8% have one to two medium-sized polyps (6-9 mm), and about 4% have lesions 10 mm and larger that are referred for immediate polypectomy.
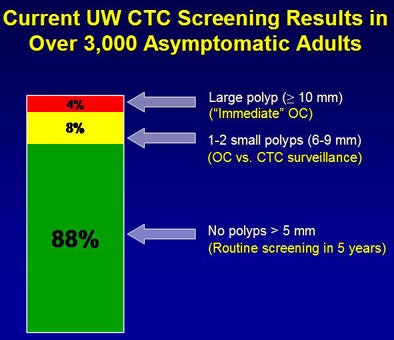 |
| Results from the first 3,000 VC screening patients show that approximately 80% have a negative exam result, 8% have one to two medium-sized polyps with the choice of polypectomy or surveillance, and 4% have positive findings that are referred for same-day colonoscopy. |
Even in this population there are lesions worth detecting, Pickhardt said. These days sensitivity can't be assessed directly inasmuch as not all patients go on to colonoscopy. But in terms of overall efficacy, the positive predictive value shows that VC appears to be just as good as finding the target lesions as colonoscopy, less invasively and far more cost-effectively, he said.
Toward this end, Dr. David Kim, Pickhardt's colleague at the university, is evaluating patients who chose first-line VC screening versus colonoscopy, Pickhardt explained. In more than 4,000 patients so far (2,000-plus in each arm) the results show that VC is finding approximately the same number of advanced adenomas and carcinomas as primary colonoscopy screening, in a population with nearly identical demographics.
The difference is that VC is finding those target lesions with about seven times fewer polypectomies than the alternative approach, sending 7% of patients on to colonoscopy rather than 100%.
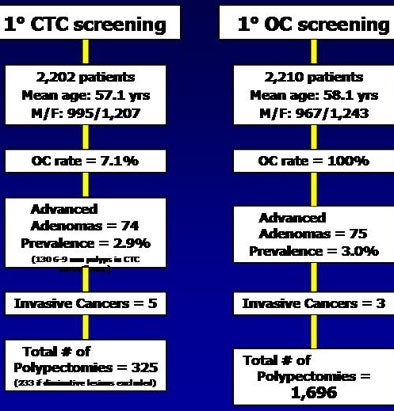 |
| Results from 2,202 VC screening subjects versus 2,210 who chose first-line conventional colonoscopy show a similar yield of advanced adenomas and carcinomas in both methods. However, the colonoscopy-first algorithm required approximately seven times as many polypectomies to achieve the same, and at a cost of three to five times as much as VC per exam. |
Even accounting for approximately 130 patients in surveillance who may eventually need colonoscopy, "I think this shows that VC is really an effective filter showing who needs colonoscopy, who benefits from it and who probably doesn't -- because we're getting at the same end results which I think is very important,' Pickhardt said.
Getting there
As for the rest of the U.S., payor acceptance of virtual colonoscopy screening can be enhanced first and foremost by producing a quality product, he said. Centers of excellence where quality control and high-quality exams cohabitate could potentially provide an early entry for some providers into reimbursed screening with VC.
"You might ask if we should demand a proven (VC) screening method," Pickhardt said. If the National CT Colonography Trial (ACRIN 6664) has good results we can assume a mix of approaches will work well, he said. If the trial falls short of expectations, "we have to go back to the drawing board and ask what meets this level of performance."
Quality-control programs will also be critical for earning payors' confidence, including elements such as referral of certain VC patients for a conventional colonoscopy exam to keep track of VC performance standards. Track positive and false-positive rates as mammographers do "just to make sure you're not out of bounds," he said.
Right now VC is being used mostly as a problem-solver, "but the holy grail is screening, and it has enormous potential for preventing cancer, and for our practices this could mean a huge area of growth," Pickhardt said. "It's a very effective filter for selecting who needs colonoscopy and who doesn't, (providing) much more effective use of a costly and invasive resource that's limited, I think."
By Eric Barnes
AuntMinnie.com staff writer
October 18, 2006
Related Reading
VC finds early niche in screening, September 27, 2006
Medicare changes, joint meetings spell progress for VC, September 4, 2006
VC finds risky polyps, might reduce polypectomies, June 8, 2006
Gastroenterologist surveys target lesions, VC practice, March 20, 2006
VC would raise screening costs, study concludes, October 31, 2005
Group credits 3D reading for best-ever VC results, October 15, 2003
Copyright © 2006 AuntMinnie.com