CHICAGO - Hypovascular liver lesions are better visualized at lower photon energies in dual-source CT (DSCT), say researchers from New York City. Attenuation differences are greater between metastases and normal liver parenchyma at 80 kVp versus weighted average data simulating 120 kVp, they concluded. Detection sensitivity was slightly lower at 80 kVp, however, owing to the smaller field-of-view on the first-generation DSCT scanner used in the study.
Dual-source CT is getting a lot of attention these days for the value it adds to abdominal imaging protocols, particularly in its ability to generate so-called "virtual noncontrast" images that add a simulated noncontrast image to the radiologist's diagnostic arsenal without the need for additional scans in multiphase image acquisition.
"There are a lot of potential benefits when evaluating dual-source CT in the abdomen," said Dr. Michael Macari, associate professor of radiology at New York University Medical Center. "We get a weighted-average dataset and you can look up purely 80-kVp images, though purely 140-kVp images probably don't have much of a role," he said. "Virtual noncontrast images are certainly a major advantage of using dual-source CT in the abdomen... You get a lot of added value and, ultimately, reduce the radiation to the patient. And, of course, you can do iodine overlays and evaluate the material composition."
Images acquired at 80 kVp have been shown in many cases to help improve conspicuity in the liver, Macari said. Vessels are seen more clearly due the k-edge effect on the iodine at 80 kVp as opposed to the weighted average images. And endovascular leaks may also be easier to see for the same reason.
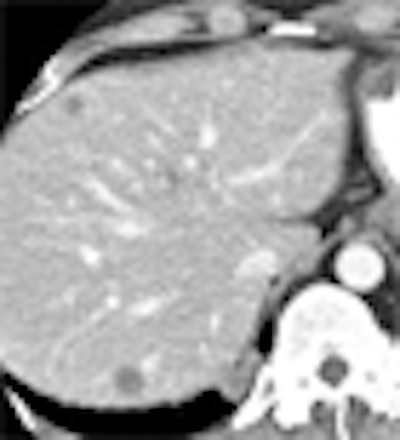
The researchers sought to determine whether the attenuation difference between normal liver and hypovascular metastases is increased at 80 kVp, when compared to weighted average data simulating 120 kVp.
 |
| Hypovascular liver lesions at DSCT are more conspicuous at 80 kVp (top) than at weighted-average data simulating 120 kVp. Images courtesy of Dr. Michael Macari. |
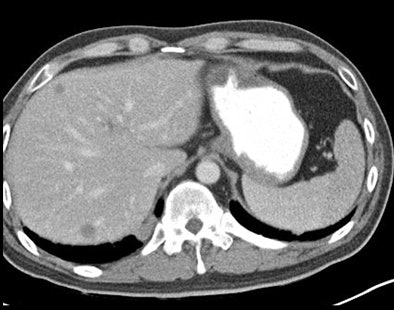 |
"Our hypothesis was that utilizing dual-source CT in the assessment of purely 80 kVp images would increase attenuation differences and the conspicuity between hypovascular metastases and adjacent liver parenchyma when compared to the weighted-average dataset, and this analysis was done with portal-venous phase imaging," Macari said Wednesday at the RSNA meeting.
Dr. Emma Robinson, Macari, and colleagues began with 286 outpatients who underwent abdominal CT utilizing a 64-detector-row dual-source, dual-energy MDCT scanner (Somatom Definition, Siemens Healthcare, Malvern, PA). The liver metastases were related to pancreatic cancer in most patients but also were related to colon cancer and breast cancer.
"We used the older-generation Siemens [Definition] system where you have two tubes operating at different kVp and mAs [settings], and one of the main limitations of this scanner is the smaller field-of-view, which is only 26.5 cm," he said.
All data were acquired with tube A operating at 140 kVp-80 mAs and tube B at 80 kVp-460 mAs. The x-ray tube was turned on 80 seconds after the injection of 1.5 mL/kg of IV contrast injected at 3-4 mL per second.
Images were reconstructed as a weighted average of the 140 kVp and 80 kVp acquisitions, simulating 120 kVp; and as pure 80 kVp data. The CT reports were reviewed, revealing 13 patients (mean age, 62 years) with 44 hypovascular liver metastases, all proven based on growth or new appearance, or confirmed on follow-up imaging.
The researchers calculated the mean attenuation of the metastasis and normal liver based on regions of interest, performing a mixed-model two-way analysis of variance to determine if the attenuation difference was significantly greater than the difference in energies.
The cases were retrospectively evaluated to determine if lesions could be seen on one or both datasets. And because the 80-kVp tube has a smaller detector than the 140-kVp tube on the old scanner model, they also noted whether any of the liver lesions were not included on the 80-kVp dataset.
The mean size of the metastases was 2.6 cm. The mean standard deviation of the attenuation difference between the metastases and the normal liver at 80 kVp was 72.3 ± 27 HU at 80 kVp versus 54.2 ± 18.7 at 120 kVp. The mean attenuation difference was significantly higher at 80 kVp (p < 0.001). In two cases, metastases were detected only at 80 kVp.
"We also noted that the attenuation of the normal liver was greater at 80 kVp [132.1 ± 19.6 HU] than at 120 kVp [100 ± 14.3 HU], and it's this difference in the attenuation of the normal liver that really tells you the difference between normal liver and the metastasis," Macari said.
Two metastases were seen only at 80 kVp, "but we did miss several lesions because of the smaller field-of-view," Macari said. "But that problem will not be an issue with the second-generation scanner."
The contrast-to-noise ratio was greater at 80 kVp even though these are noisier images, because the contrast is so much greater.
"This is an evolving technology with the use of dual-energy imaging, but the use of 80-kVp images has the potential to enhance differences between hypovascular metastases and normal liver by enhancing the attenuation differences." Limitations included the retrospective design of the study and the small population studied, he said.
Pure 80-kVp data acquired from a DSCT scanner demonstrate greater attenuation differences between metastatic disease and normal liver, potentially improving the assessment of early metastatic disease, Macari said.
By Eric Barnes
AuntMinnie.com staff writer
December 3, 2009
Related Reading
CT of colorectal liver mets may predict survival, December 1, 2009
Evidence scarce to support RF ablation of colorectal CA metastases in the liver, November 17, 2009
Perfusion CT predicts tumor response to antiangiogenic treatment, December 1, 2008
ROI changes colorectal tumor perfusion measurements, August 26, 2008
Copyright © 2009 AuntMinnie.com