While biopsy remains the final diagnostic procedure for suspected breast cancer, Japanese researchers have suggested that multidetector CT (MDCT) may warrant a larger role in earlier detection and surgical planning.
In their study of 147 women, MDCT depicted the tumor invasion of invasive lobular carcinoma more accurately than mammography or sonography, according to researchers from the Kinki University School of Medicine.
"MDCT data were the basis for a change in surgical methods in six of the 147 patients. Breast conservation surgery was changed to mastectomy for four patients. For the other two patients, additional lesions detected on MDCT required local excision," the researchers wrote in the American Journal of Roentgenology (September 2003, Vol. 181:3, pp. 679-686).
The researchers detected 173 breast lesions during their study. They used an Aquilion scanner (Toshiba Medical, Tokyo) and imaged patients before and after a bolus injection of nonionic contrast (Omnipaque [iohexol], Daiichi Pharmaceutical, Tokyo). One radiologist compared the MDCT images with those from mammography and sonography; histologic findings served as the gold standard.
As part of their analysis, the researchers also looked for potential indicators of malignancy among the tumors seen. Not surprisingly, an irregular shape was highly indicative of malignancy -- 99% of tumors with irregular shape were malignant versus just 67% with other shapes, a highly significant finding (p < 0.0001).
A similar difference was found for masses with homogeneous or rim enhancement versus heterogeneous enhancement, with carcinoma found in 95% of the former versus 63% of the latter (p < 0.0001).
One difference between MDCT and mammography was that the spiculated margins seen on MDCT had a positive predictive value for malignancy of 99%, substantially higher than the 70%-80% rate among those detected mammographically.
"This result may be explained by the fact that MDCT can depict the mass margin accurately without overlapping other tissues," the authors wrote. "In contrast, 45% of smoothly marginated masses that we studied were malignant."
However, a smooth margin wasn’t a reliable indicator of benignity on MDCT, the researchers found. Their MDCT findings included three mucinous carcinomas and one medullary carcinoma with smooth margins.
The incidence of malignancy among the study’s nonmass enhancing lesions was 91%, higher than the 67%-86% for MRI-detected lesions reported in previous studies. The researchers speculated that this higher malignancy incidence might be related to the low proportion of fibrocystic disease in their study.
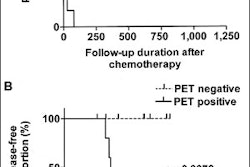
The researchers also looked at the positive predictive values of the time-density curve, and found the washout and plateau patterns to be predictive at 95% and 85%, respectively, while the persistent pattern, at 58%, was not. However, since other tumor characteristics were more predictive and the time-density curve analysis involves more radiation exposure for the patient, the researchers said they don’t routinely use such analyses at their institution.
Overall, MDCT of the breast can be used to predict the presence of breast cancer with an accuracy of 90%, the authors concluded. The modality’s major downside, according to the authors, is its radiation burden. The skin radiation dose measured by the researchers during a single breath-hold acquisition was 26 mGy, around 10 times higher than the dose received during standard mammography.
The group's next step will be to compare MDCT to MRI of the breast, which is also reported to be more accurate than mammography and sonography. Only one comparison of helical CT and MRI has been published to date, they wrote, with helical CT performing almost as well as MR mammography for assessment of the extent of breast cancer.
MDCT also has several advantages over MRI, including its facilitation of simultaneous evaluation of axilla lymph nodes and lung metastases. Wrote the authors: "With MDCT, the breast can be scanned faster and with thinner collimation than is possible with MR mammography and the patient can be supine, allowing a surgical simulation for breast conservation using a three-dimensional display and an easy approach for CT-guided breast biopsy."
By Tracie L. ThompsonAuntMinnie.com contributing writer
September 17, 2003
Related Reading
Contrast digital mammography helps visualize cancer in dense breasts, August 29, 2003MRI useful in detecting missed breast cancer in high-risk women, June 25, 2003
Effective breast CAD still harbors a few workflow caveats, June 3, 2003
Strict attention to detail enhances sensitivity of breast US, April 17, 2003
Copyright © 2003 AuntMinnie.com