With multidetector-row CT being used increasingly for virtual colonoscopy exams, researchers are eager to find out if the technology’s prowess in other applications will translate to higher sensitivity and specificity in colorectal cancer detection.
The question is difficult to answer clinically, since any direct comparison of single- vs. multislice techniques would require subjects to be scanned twice. Moreover, any number of variables such as reader experience, CT parameters, interpretation methods, and prep quality, are known to affect accuracy regardless of detector configuration.
What is certain is that the zippy new scanners continue to win friends and influence people. Researchers at the University of Rome recently produced excellent virtual colonoscopy results at low radiation doses on a four-slice machine. Japanese investigators are crediting their 16-slice scanner with helping them detect flat lesions.
At the 2003 European Congress of Radiology in Vienna, Dr. Alice Gillams from Middlesex Hospital in London presented a study of multidetector-row CT virtual colonoscopy in 139 symptomatic elderly subjects. In a presentation at the 2002 RSNA meeting in Chicago, Dr. Hiro Yoshida put both MDCT and SDCT to the test with a computer-aided detection scheme. For both groups, the multislice protocols yielded excellent results.
Published literature for single-slice CT has shown sensitivities as high as 91% for polyps 10 mm and larger, dropping as polyps get smaller, Gillams said. "We wanted to see whether the advantages of multislice, with which we are all very familiar -- the improved spatial resolution, the improved temporal resolution, and improved reformat -- can aid our interpretation of CT colonography."
To that end, Gillams and colleagues imaged 139 elderly patients (mean age 70, all symptomatic with suspected colorectal cancer) using a four-slice scanner, using 1-mm collimation, 1.5-mm reconstruction, 4 x 2.5-mm beam collimation, and table speed of 17.5 mm/sec.
Using a technique somewhat different from the norm, intravenous contrast was routinely administered before imaging and after standard bowel preparation. "We give 100 to 150 ml of Omnipaque 300 at 5ml/sec," Gillams wrote in an e-mail to AuntMinnie.com. "We scan from the pelvis to the diaphragm after a 30-second delay. This means you reach the inferior surface of the liver at about 50 seconds (during the) portal venous phase, the optimal time to detect hypoattenuating colorectal metastases. Therefore, one procedure detects and stages," she wrote.
A previous study at her institution found that results in high-risk patients were much better using contrast, Gillams said in her presentation.
The image acquisition differed slightly too, in that patients generally underwent only supine imaging, supplemented by prone exams only when they were needed to answer diagnostic questions. The technique saves time and radiation dose, she said.
"We have measured attenuation values in polyps and cancers both before and after IV contrast, and have (found) that both polyps and cancers enhance vividly," Gillams explained in her e-mail. "Therefore it is possible to detect a polyp with a contrast study even if it is surrounded by fluid. This reduces the need for both supine and prone imaging as the fluid residue is no longer a problem. If there is a lot of solid residue or non-optimally distended segments, we still perform both supine and prone."
To correlate the results, all of the patients underwent same-day conventional colonoscopy as a reference standard. The data were evaluated using axial images, multiplanar reformats, and occasionally 3-D reconstructions when the first two methods were inconclusive.
Of 57 total cancers detected, virtual and conventional colonoscopy each found 56. "In terms of polyps, we detected all of our polyps over 10 mm, we detected 7 of 9 polyps between 6 and 9 mm, and we didn't do very well in the small-polyp range, below 5 mm (9/26, 35%)," Gillams said.
In virtual colonoscopy's favor, 39 of 139 conventional colonoscopies could not be completed; 30 of these involved distal occlusive cancer, Gillams said. In addition, conventional colonoscopy missed one cecal carcinoma and one 15-mm rectal polyp. However, MDCT virtual colonoscopy missed a 9-mm cancer that remained occult on retrospective review.
"This is the false-negative, a 9-mm Dukes A carcinoma in a length of sigmoid diverticulitis," she said. Unfortunately, the cancer remained undetectable using any type of image reconstruction. Even with prior knowledge of its presence, it could not be visualized in the typically low-attenuating diverticular wall of the stenosed segment.
 |
| Above, axial CT image (left) and curved reformat (right) shows severe stenosing diverticular disease. Within this area was a 9-mm Dukes A carcinoma, not detected as a distinct lesion on CT, but found on histology. Image courtesy of Dr. Alice Gillams. |
In another case, a false-positive virtual colonoscopy result, a mass was correctly suspected of being a prominent iliocecal valve, but endoscopic correlation was needed to be sure. Also, overall sensitivity remained low for polyps under 5 mm, giving rise to difficult questions regarding follow-up, Gillams said.
"We've gotten to the point now where it's almost like tossing a coin," Gillams said of managing the elderly patients' care. "Is it more detrimental to subject patients to colonoscopy because you've called a false-positive on a tiny polyp which is unlikely to be clinically important, or is it better to not even get into that discussion and try not to diagnose the very tiny polyps?" For her part, Gillams said she tries not to diagnose very small polyps on virtual colonoscopy unless she can see that the colon is very clean.
"We felt that multislice is better than the single-slice data, and the next step really is to obviate the need for bowel preparation, and to reduce the radiation dose," she concluded.
In comparison of CAD groups, multislice prevails, slightly
At the 2002 RNSA meeting in Chicago, Dr. Hiro Yoshida from the University of Chicago took another tack, presenting a study that compared single-detector CT results in one group of virtual colonoscopy subjects to MDCT results in another. The retrospective analysis examined the performance of computer-aided polyp detection in both groups.
"The purpose was to assess the performance of the group's CAD scheme for detection of polyps in CTC based on two independent databases for polyps," Yoshida said.
A total of 44 cases were examined retrospectively, 22 of which had been acquired using a single- slice HiSpeed CT/i CT scanner (GE Medical Systems, Waukesha, WI), and 22 cases that had been imaged on a multislice scanner, a GE LightSpeed QX/i.
All of the scans had been performed using 2.5- to 5-mm collimation, 1.5- to 2.5-mm reconstruction intervals, and tube currents ranging from 60 to 110 mAs.
All of the cases were processed using the group's CAD scheme, and the results were analyzed using discriminant analysis and leave-one-out evaluation "in which all but one polyp candidate were considered," to test the results, Yoshida said.
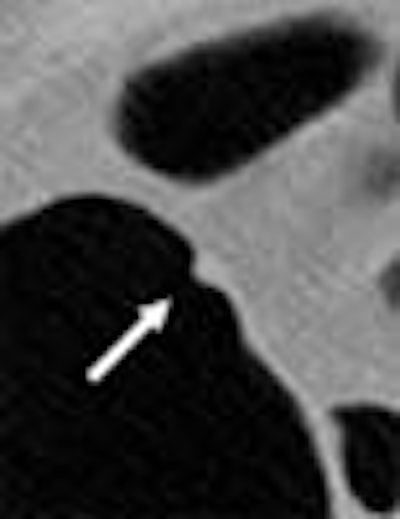
 |
| Above, a 7-mm sessile polyp (arrow) in the sigmoid colon imaged by a single-detector CT scanner. (a) Transverse image, (b) coronal image, (c) endoluminal view with volume rendering, and (d) endoluminal view color-coded based on the output of CAD, in which the polyp is highlighted by green. The shape of the polyp is fuzzy and blurred, especially in the coronal image, and as a result it was hard to detect using CAD. Images courtesy of Dr. Hiro Yoshida. |
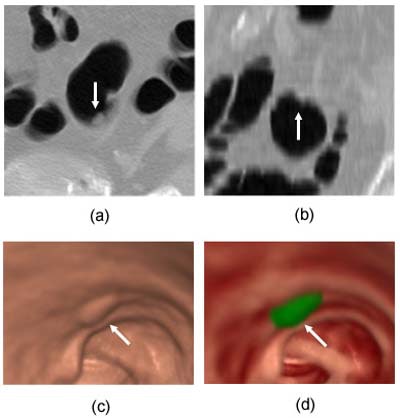
 |
| Above, a 5.3-mm sessile polyp (arrow) in cecum imaged by a four-row multidetector CT scanner. (a) Transverse image, (b) coronal image, (c) endoluminal view with volume rendering, and (d) endoluminal view color-coded based on the output of CAD, in which the polyp is highlighted by green. The polyp is clearly delineated in both transverse and coronal images as well as in the endoluminal view, and thus it was easily detected by CAD despite its small size. Images courtesy of Dr. Hiro Yoshida. |
The application of CAD yielded 100% sensitivity (by patient) in both databases. However, single-detector CT yielded 1.6 false positives per patient, while MDCT produced only 0.9 false positives per patient. By-polyp sensitivity was 95% for MDCT, and lower for the single-detector scanner, he said.
 |
| Above, CAD results show fewer false-positives using MDCT. Chart courtesy of Dr. Hiro Yoshida. |
In ROC analysis for the discrimination of true from false positives, Az values were 0.95 and 0.93 for MDCT and SDCT, respectively. Thus, the use of multidetector-row CT could potentially improve polyp detection in virtual colonoscopy, Yoshida concluded.
By Eric BarnesAuntMinnie.com staff writer
May 2, 2003
Related Reading
Colon CAD finds complementary role with radiologists, April 23, 2003
Ultralow-dose virtual colonoscopy shows high sensitivity, April 8, 2003
Thin slices, narrow collimation rule in virtual colonoscopy study, March 8, 2003
Virtual colonoscopy aces first flat-lesion study, December 3, 2003
Copyright © 2003 AuntMinnie.com