Amid questions about its methodology, the largest virtual colonoscopy trial to date has yielded preliminary data that are far poorer than the results of previous studies.
According to early data from nearly 600 patients in the trial, virtual colonoscopy yielded just 44% overall sensitivity for the detection of colorectal polyps 10 mm and larger, with 40% sensitivity for polyps 6 mm and larger. In previous virtual colonoscopy studies, sensitivities have ranged from 80% to 92% for similarly large neoplasia, and from 75% to 82% for medium-sized polyps.
The lead investigator, gastroenterologist Dr. Peter Cotton from the Medical University of South Carolina (MUSC) in Charleston, NC, presented the early results of the trial at the Digestive Disease Week meeting on May 22 in San Francisco.
The study, coordinated by MUSC's Clinical Innovation Group and funded by the U.S. Department of Defense, was hailed as the largest virtual colonoscopy study to date, and the first multicenter trial to compare conventional colonoscopy to the virtual kind. Nine centers participated in all, including 8 in the U.S. and 1 in the U.K.
The study population consisted of 600 patients, over age 50, who were scheduled for a clinically indicated conventional colonoscopy.
The subjects underwent standard bowel prep with 3 ounces of oral sodium phosphate solution in two equal doses. Patients with congestive heart failure and renal failure were excluded due to use of the saline prep.
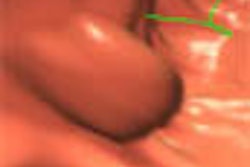
Following bowel insufflation with either room air or CO2, the patients underwent noncontrast virtual colonoscopy on multislice (quad) spiral CT scanners in both prone and supine positions. The CT scanner settings were as similar as possible owing to different scanner models in the participating centers, and generally included 4 x 5-mm slices, pitch of 3, and 1-mm reconstruction intervals.
VC was followed by same-day conventional colonoscopy, using the same prep. Initial radiology reports were given on the two-dimensional CT images, and reconstruction fly-throughs were reviewed at a later date. Each center was limited to 3 endoscopists and 2 radiologists. The latter were required to have performed at least 10 virtual colonoscopies before beginning the trial.
"The true polyp status, that is the gold standard that is used in this study, is clearly biased towards colonoscopy," Cotton said. True polyp status consisted of the initial colonoscopy results, plus any new colonoscopy findings following review of virtual colonoscopy results, plus any other findings resulting from follow-up exams or surgery.
"Very importantly, the colonoscopist was initially blinded to the results of the virtual colonoscopy," Cotton said. "But in order to double-check any discrepancies, the findings of VC were revealed to the colonoscopist sequentially during withdrawal of the endoscope, to allow for examination of (each) segment."
Thus, as soon as the endoscopist completed a colon segment, he or she opened an envelope containing the VC results. Any additional findings could then be reexamined endoscopically before proceeding to the next colonic segment.
According to the results, "virtual colonoscopy identified only 18 of 41 subjects with polyps greater than or equal to 10 mm, that's 44% (sensitivity)," Cotton said. "When we get down to polyps 6 mm or more, we're down to 40%. Specificity was high."
Results by polyp showed 55% sensitivity for polyps 10 mm or larger, and 33% for polyps 6 mm or larger, he said. Eight cancers were found, of which virtual colonoscopy missed 2: a 17-mm rectal lesion, and a 7-mm tumor in the ascending colon. The only complication was minor self-limited bleeding resulting from colonoscopy in one patient.
Interestingly, the center with the most experience, 188 patients, identified 20 of 24 subjects (83%) with polyps 6 mm and larger, certainly an acceptable figure, Cotton said. But other high-volume centers performed much worse.
"It's obvious that the overall sensitivity (of virtual colonoscopy) is not adequate for general applications, at the least in the centers in which it's being evaluated today," Cotton concluded. "The results vary enormously between centers, and one of the most important things that remains to be done is to analyze why the results are so different between different centers. It may be that many of our radiologists were not sufficiently experienced, and that the results might be different with greater experience. I believe that virtual colonoscopy is still a very interesting potential technique, but we need to look at expertise and improved training techniques before it can be used in general practice."
An audience member questioned whether 10 virtual colonoscopies really constituted enough experience to perform VC properly, and Cotton said that experience was one of the factors that would certainly be evaluated before the MUSC study was published.
"Obviously the results were disappointing, but they are still somewhat preliminary," Cotton wrote in an e-mail to AuntMinnie.com. "Although all but 20 data sheets have been validated and analyzed, we do need to see the results of the later fly-throughs. In addition, we are getting more information about the precise experience of the radiologists, and (we are) analyzing the results to see if we can find any common factors for accuracy/inaccuracy, and whether there is an improvement over time. I would like to get all the radiologists together to chew over the data, and hope this may be possible."
Dr. Matthew Barish, assistant professor of radiology with the Boston Medical Center, wrote AuntMinnie.com to say that one has to be very cautious when interpreting preliminary results, but that the study’s methodology seemed inadequate.
"Radiologists involved in this technique understand the learning curve, as well as the multiple technical factors that can impact the results of such a study," Barish wrote. "The training and experience of the VC readers will have had a tremendous impact on the results. I am sure the study designers would not have considered allowing gastroenterologists who had performed only 10 fiber-optic (video-assisted) colonoscopies to participate in the study. Also, the VC readers were hamstrung by only (being able to) review the 2-D images without 3-D for problem solving. Two- and three-dimensional integrated reading should be considered the minimum for interpretation of VC studies."
And in the event patients were poorly prepped or distended, those factors alone could have explained the poor results, he added.
"I think my conclusions are fair based on the current data," Cotton wrote. "They provide a useful counterpoint to the current published data, virtually all of which comes from single centers and enthusiastic radiologists."
Dr. Abraham Dachman, CT director at the University of Chicago, said the per-polyp data should have been worse than the per-patient data, and the fact that MUSC reported the reverse suggests that the statistic should be recalculated from scratch.
"Knowledge of the steep learning curve was widely known among experts for several years," Dachman wrote. "In planning such an important multicenter trial, strict training criteria and ongoing unblinding of the radiologists should have been instituted."
Dr. Joseph Ferrucci, radiology department chair at the Boston University School of Medicine, saw a pattern. "Whenever gastroenterologists have controlled comparative studies of colon polyp imaging, radiology comes out poorly," he wrote to AuntMinnie.com. "When radiologists control imaging studies, results are better and more consistent among radiology researchers."
By Eric BarnesAuntMinnie.com staff writer
June 3, 2002
Copyright © 2002 AuntMinnie.com