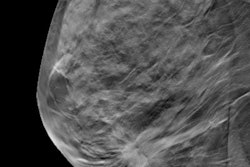
Digital breast tomosynthesis (DBT) may be the best option for categorizing possibly benign lesions in women with a personal history of breast cancer, according to research published April 12 in the American Journal of Roentgenology.
A team led by Lily Offit from Harvard Medical School found that compared with full-field digital mammography (FFDM), DBT showed a significantly higher frequency and lower malignancy rate for BI-RADS 3 assessments, as well as a higher malignancy rate for BI-RADS 4 assessments.
"Our findings support the use of DBT, including in patients with a history of breast cancer," said corresponding author Dr. Sona Chikarmane from Brigham and Women's Hospital to AuntMinnie.com.
BI-RADS 3 lesions have a malignancy rate of 2% or less, according to previous studies. Women in this category are recommended to undergo short-interval follow-up imaging at six, 12, and 24 months, which could add stress or be a financial burden.
The researchers pointed out that with DBT's use on the rise, BI-RADS 3 assessments have reduced relative to FFDM, with calcifications being the main mammographic finding.
Women with a personal history of breast cancer are at risk for recurrent or second breast cancers. Previous research suggests that DBT may lead to lower recall rate and a lower rate of false-positive findings in these women. The researchers wrote that due to these women having an increased relative risk for breast cancer, assessing for BI-RADS 3 cases here "demands special consideration."
Offit and co-authors wanted to compare the frequency, outcomes, and additional characteristics of BI-RADS category 3 assessments between FFDM and DBT in women with a personal history of breast cancer.
They looked at retrospective data from 14,845 mammograms in 10,118 women with an average age of 61.8 years, all of whom had a personal history of breast cancer and had undergone mastectomy or lumpectomy. Out of the total, 8,422 exams were performed by FFDM from 2014 to 2016, and 6,423 exams were performed by FFDM with DBT from 2017 to 2018. The latter followed interval conversion of the center's mammography units.
The researchers found that DBT led to lower frequency of BI-RADS 3 assessment and lower malignancy rate for such lesions compared with mammography.
| Comparison between DBT, full-field digital mammography | |||
| Mammography | DBT | p-value | |
| Frequency of BI-RADS 3 assessment | 6.4% | 5.6% | 0.05 |
| Malignancy rate for BI-RADS 3 lesions | 5.0% | 1.8% | 0.04 |
| Malignancy rate for BI-RADS 4 lesions | 23.2% | 32.0% | 0.03 |
| Malignancy rate for BI-RADS 5 lesions | 75% | 100% | 0.02 |
The researchers also analyzed index category 3 lesions, which included 438 lesions for FFDM and 274 for DBT, respectively. They reported that DBT had a lower percentage of biopsied lesions with a malignant diagnosis compared to mammography, 13.9% to 36.1% (p = 0.02). Additionally, DBT showed more frequent mammographic finding type of mass compared to mammography, 33.2% to 23.1% (p = 0.003).
Chikarmane said that these results may be because there is a greater conspicuity of benign-appearing masses on DBT than on digital mammography.
"The interpreting radiologist may have recommended follow-up imaging for these benign-appearing masses due to the concern for second cancers in patients with a personal history of breast cancer and an associated abundance of caution," she told AuntMinnie.com.
The study authors suggested that these insights could help in establishing whether BI-RADS 3 assessments in these women are within benchmarks for early detection of second cancers and reduction of benign biopsies.
"The study's findings have clinical relevance given the inclusion of BI-RADS category 3 assessment in the basic clinical audit in the upcoming edition of the BI-RADS manual," the authors wrote.
Chikarmane added that more research will be needed on BI-RADS 3 usage in all patient populations, including those using MRI and ultrasound.