A woman's age may predict whether an interval breast cancer will have a poor outcome better than her breast density, according to a research letter published online May 3 in JAMA Oncology. The finding could direct the use of supplemental screening in women.
When it comes to catching interval breast cancers, the conversation about which women should have supplemental screening has focused mainly on breast density as the primary factor, wrote a team led by Anne Marie McCarthy, PhD, of Massachusetts General Hospital. But it may be more effective to consider age -- particularly for women between the ages of 40 and 49 -- as well as breast density to identify those at risk of breast cancer who might have a poor prognosis.
"Although breast density is predictive of interval cancer overall, it is less predictive of whether that interval cancer will have a poor prognosis," the group wrote. "Younger age is predictive of interval breast cancer with a poor prognosis. This may reflect the dual origins of interval cancers."
Predicting prognosis
Interval cancers are those that were present at a woman's last screening mammography exam but not caught, as well as those that developed after the exam. This second category tends to include more aggressive cancers and poorer outcomes, according to McCarthy and colleagues.
"Cancers that are present but not detected by screening mammography may be more likely to be associated with a good prognosis and occur among older women, whereas cancers that develop between screening examinations may be more likely to be rapidly growing cancers associated with a poor prognosis and occur among younger women," they wrote.
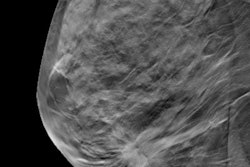
For the study, the researchers used data from the Population-Based Research Optimizing Screening Through Personalized Regimens (PROSPR) consortium, including 306,028 women 40 years and older with no earlier diagnosis of breast cancer who underwent screening mammography between 2011 and 2014. Negative mammograms were those with an initial BI-RADS category of 1 or 2; all other categories were classified as positive results. The team used state cancer registries to identify breast cancer diagnoses within one year after screening mammography.
McCarthy and colleagues defined breast cancer cases with poor prognosis by the following criteria:
- Distant metastases
- Cancer in regional lymph nodes
- Estrogen receptor-positive and/or progesterone receptor-positive and human epidermal growth factor receptor 2 (HER2)-negative invasive cancer at least 2 mm in diameter
- HER2-positive invasive cancer at least 1 cm in diameter
They then evaluated any association of age, breast density, and family history with cancer diagnosis using odds ratios. A ratio greater than 1 pointed to higher odds of a particular outcome, a ratio of 1 to no association, and a ratio less than 1 to lower odds of a particular outcome.
McCarthy and colleagues found that cancers diagnosed after negative screening mammography were more likely to have poor prognoses (43.8%) than those diagnosed after positive mammography (26.9%). Women with dense breast tissue were twice as likely to receive a cancer diagnosis -- regardless of prognosis -- than women who did not have dense tissue.
The group also found the following:
- Among women who received a diagnosis of cancer after negative screening mammography, those between the ages of 40 and 49 were more likely to have poorer prognoses than women 70 and older (odds ratio, 3.52; p = 0.048).
- For women with positive mammography results, younger women had lower odds of a cancer diagnosis than older women (odds ratio, 0.22; p = 0.001), but those with a family history of the disease had higher odds (odds ratio, 1.29; p = 0.001).
- For women ages 40 to 49 with negative mammography results, their age was not significantly associated with breast cancer diagnosis, compared with women 70 and older (odds ratio, 0.81; p = 0.6).
- For women with negative screening mammography, breast density and family history were not significantly associated with poor prognosis (breast density: odds ratio, 0.6; p = 0.3; family history: odds ratio, 0.8; p = 0.65).
"Our results indicate that the positive predictive value of mammography results depends on patient age and family history," the group wrote. "In contrast, the negative predictive value depends on breast density but not on patient age or family history."
Targeted screening
Identifying women who are at high risk of breast cancer with poor prognosis despite regular mammography could help clinicians develop targeted, additional screening, according to the authors.
"Although the rate of breast cancer after negative mammography results is small, the likelihood that such cases will be associated with a poor prognosis highlights the need to improve early detection for these women," they concluded.