Low-dose positron emission mammography (PEM) can detect invasive breast cancer in a feasible manner, according to research published February 9 in Radiology: Imaging Cancer.
A team led by Vivianne Freitas, MD, from the University of Toronto found that PEM performed comparably to MRI in breast cancer detection and could serve as a supplemental imaging method for evaluating dense breasts.
"This groundbreaking imaging technique presents a compelling alternative, mirroring the clinical utility of traditional mammography and MRI but utilizing considerably lower doses of radiation when compared with previously molecular breast imaging," Freitas told AuntMinnie.com. "It holds promise for screening and diagnostic applications, potentially revolutionizing how radiologists approach breast cancer detection."
While conventional mammography remains the gold standard in breast cancer screening, its performance suffers when imaging dense breasts. This is where supplemental imaging such as MRI and molecular breast imaging come into play.
PEM is one molecular breast imaging method that has shown promise in lowering the number of false-positive cases, owing to its superior specificity over MRI. However, PEM’s higher radiation dose has steered radiologists away from using the modality.
Freitas and colleagues investigated the feasibility of low-dose PEM and compared its performance to that of MRI in identifying breast cancer, as well as determining the local extent of cancers found.
For the study, the researchers utilized PEM with up to 185 MBq of F-18-labeled fluorodeoxyglucose (F-18 FDG). Two breast radiologists who had no prior knowledge of cancer location reviewed PEM images taken one and four hours following F-18 FDG injection. The team also correlated findings with histopathologic results.
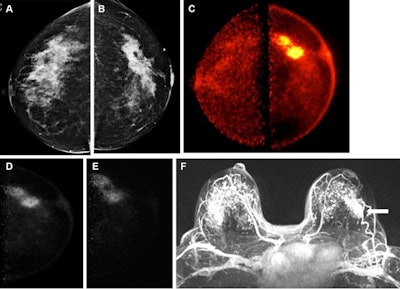 Images obtained in a 50-year-old female patient with a new biopsy-proven malignant lesion in the left breast. (A) Craniocaudal mammogram of the right breast does not show any lesion. (B) The malignant lesion corresponds with a 7-cm irregular and spiculated mass on the left craniocaudal mammogram. Ultrasound-guided core-needle biopsy revealed grade 2 invasive lobular carcinoma. (C) The bilateral positron emission mammographic craniocaudal color image obtained one hour after intravenous injection of 185 MBq of F-18-labeled fluorodeoxyglucose (F-18 FDG) shows a mass with intense uptake in the left breast with known cancer and no abnormal uptake in the right breast. Positron emission mammographic craniocaudal images of the left breast obtained (D) one hour and (E) four hours after intravenous injection of 185 MBq of F-18 FDG show no substantial visual difference in uptake of the known cancer. (F) Axial contrast-enhanced fat-saturated subtracted T1-weighted MR image with maximum intensity projection reconstruction obtained 90 seconds after intravenous injection of 0.1 mmol of gadolinium-based contrast material per kilogram of body weight also shows the enhancing mass corresponding to known malignancy (arrow) and marked bilateral background parenchymal enhancement, with multiple nonspecific foci of enhancement in the contralateral breast. The patient opted for bilateral mastectomy, which confirmed left-sided malignancy and no malignancy in the contralateral breast. Image courtesy of the RSNA,
Images obtained in a 50-year-old female patient with a new biopsy-proven malignant lesion in the left breast. (A) Craniocaudal mammogram of the right breast does not show any lesion. (B) The malignant lesion corresponds with a 7-cm irregular and spiculated mass on the left craniocaudal mammogram. Ultrasound-guided core-needle biopsy revealed grade 2 invasive lobular carcinoma. (C) The bilateral positron emission mammographic craniocaudal color image obtained one hour after intravenous injection of 185 MBq of F-18-labeled fluorodeoxyglucose (F-18 FDG) shows a mass with intense uptake in the left breast with known cancer and no abnormal uptake in the right breast. Positron emission mammographic craniocaudal images of the left breast obtained (D) one hour and (E) four hours after intravenous injection of 185 MBq of F-18 FDG show no substantial visual difference in uptake of the known cancer. (F) Axial contrast-enhanced fat-saturated subtracted T1-weighted MR image with maximum intensity projection reconstruction obtained 90 seconds after intravenous injection of 0.1 mmol of gadolinium-based contrast material per kilogram of body weight also shows the enhancing mass corresponding to known malignancy (arrow) and marked bilateral background parenchymal enhancement, with multiple nonspecific foci of enhancement in the contralateral breast. The patient opted for bilateral mastectomy, which confirmed left-sided malignancy and no malignancy in the contralateral breast. Image courtesy of the RSNA,
The team included 25 women with a median age of 52 years in the study with a range of 32 to 85 years. On 100 sets of bilateral PEM images, 24 (96%) of 25 cancers were identified. Of the cancers found by PEM, 19 were invasive and five were in situ diseases. This showed PEM’s “comparable performance” even after three hours of radiotracer uptake, according to the researchers.
Additionally, the team reported that the median invasive cancer size was 31 mm, and PEM missed an additional three grade-2 in situ lesions.
Finally, PEM found fewer false-positive additional lesions (one of six, 16%) compared with MRI (eight of 13, 62%). However, this did not achieve statistical significance (p = 0.14).
Still, Freitas said this advancement "could profoundly affect patient care by lowering patient anxiety and decreasing the number of unnecessary biopsies and treatments."
"It represents a step forward towards a more focused and accurate approach in the medical field," she told AuntMinnie.com.
The study authors called for larger studies to validate their findings, as well as to find out what specific scenarios PEM could be most applicable in.
"If this technique confirms the preliminary results and effectively reduces false positives, it could substantially mitigate the psychological stress and anxiety that patients experience due to inaccurate results," Freitas added.
In an accompanying editorial, David Barreto, MD, and Jocelyn Rapelyea, MD, from George Washington University echoed that low-dose PEM protocols show promise as a future alternative adjunctive breast imaging tool in certain patients who may have contraindications to other imaging modalities.
“Decreasing false-positive findings can … lead to other potential benefits, such as reduced patient anxiety and overall cost burden, as additional workups and biopsies may be rendered unnecessary,” they wrote. “Another advantage of low-dose PEM is its shorter acquisition time [approximately 20 minutes] to complete the four standard views as compared with a full breast MRI protocol [approximately 30 minutes] and some protocols using MBI [between 28 and 40 minutes].”
The full study can be found here.