U.S. researchers have found that adding whole-brain radiation therapy to stereotactic radiosurgery isn't necessary for treating patients with brain metastases. In fact, adding whole-brain radiation more than doubles a patient's risk of cognitive decline compared to those who receive only stereotactic radiosurgery.
The differences in learning and memory were so significant that a clinical trial being conducted by the University of Texas M. D. Anderson Cancer Center of Houston was halted after interim analysis of the data.
"The results of this study could change the practice of how brain metastases are managed in the U.S.," radiation oncologist Dr. Eric Chang told attendees of the annual meeting of the American Society for Therapeutic Radiology and Oncology (ASTRO), held last fall in Boston.
"Treatment using whole-brain radiation therapy immediately after stereotactic radiosurgery has been controversial and the subject of intense debate," Chang said. "For this reason, we initiated a clinical trial comparing these two types of treatments."
Chang and colleagues hypothesized that patients receiving stereotactic radiosurgery (SRS) and whole-brain radiation therapy (WBRT) would have inferior neurocognitive function compared to patients who received only stereotactic radiosurgery. However, statistical analysis of a sample size of 90 patients generated a pretrial assumption that each treatment group had a mean probability of a 25% decline.
A total of 58 patients were enrolled. All had a baseline brain MRI exam and received stereotactic radiosurgery between January 2001 and September 2007. Twenty-eight of the patients also received whole-brain radiation therapy within three weeks of SRS. Eligible patients were older than 18 years with no more than three brain metastases diagnosed as recursive partitioning analysis (RPA) class 1 or 2.
Patients who had prior brain surgery or radiation therapy; whose primary cancer was unknown; or who had a diagnosis of leukemia, lymphoma, small cell lung cancer, leptomeningeal disease, or a germ cell tumor were ineligible for the trial. Pregnant patients and patients with an RPA class 3 metastasis were also excluded.
Although the patients were randomized into two groups, the groups were very similar, Chang noted. The median age of the SRS-only group was 63 years, compared with 64 for the SRS+WBRT group. In the SRS-only group, 40% of the patients were male, compared with 61% in the SRS+WBRT group. The majority of patients in each group had only one lesion (60% SRS versus 54% SRS+WBRT). The primary cancer for both groups was lung, followed by breast, melanoma, and renal.
The stereotactic radiosurgery dose was based on Radiation Therapy Oncology Group (RTOG) 90-05 guidelines:
|
Patients in the SRS+WBRT group received 30 Gy of radiation in 12 fractions of 2.5 Gy per day.
Patients were stratified according to the number of brain metastases, histology, and RPA class. Upon completion of treatment, the patients had a clinic visit, brain MRI exam, and formal neurocognitive evaluation at one, two, four, six, nine, 12, 15, and 18 months. If this schedule was completed by a patient, he or she would continue to return in six-month intervals. However, the median follow-up for the entire cohort was only 7.5 months.
The Hopkins Verbal Learning Test was used to measure decline in learning and memory by detecting a more than five-point drop four months from the baseline evaluation. The five-point drop was based on statistical and psychometric properties, and was not arbitrarily chosen, Chang emphasized. He noted that the Hopkins Verbal Learning Test is widely used and has demonstrated sensitivity to neurotoxic effects of cancer treatment.
Sharper declines with both therapies
Interim analysis showed (with a 96.4% statistical probability) that patients who underwent only SRS had a 23% decline in neurocognitive function. By comparison, patients who received both therapies had a 49% decline. Neurocognitive outcome was measured by the ability of patients to immediately recall a list of 12 words after three attempts. For patients who receive both therapies, nearly half lost the ability to recall five words from the same list over three attempts.
"Learning and memory are negatively affected to a greater degree by toxicity from initial whole-brain radiation therapy than by increasing progression of distant brain metastases resulting from omission of this therapy," he said. "Stereotactic radiosurgery alone, coupled with close clinical monitoring, is recommended as the preferred initial treatment strategy to better preserve neurocognitive functions in patients newly diagnosed with one to three brain metastases."
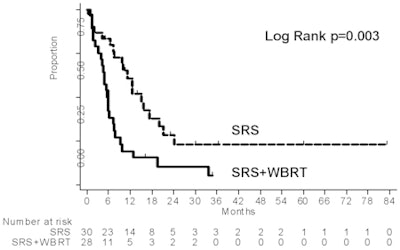
Local freedom from progression at 12 months was 100% with SRS+WBRT compared to 67% for the patients who received stereotactic radiosurgery alone. This advantage was negated by the fact that the patients who received SRS+WBRT survived a median of 5.6 months, with only 19% surviving a year or more. By comparison, the patients who received SRS survived an average of 15.2 months, with 61% surviving a year or more.
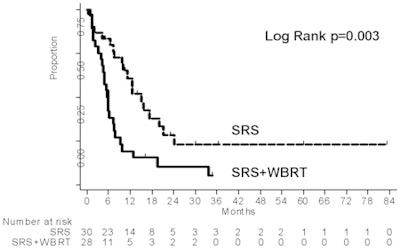 |
| Image provided with permission of Dr. Eric Chang. |
Surprised by the excellent survival results for SRS alone, the researchers hypothesized that intense follow-up and aggressive early salvage therapies with the stereotactic radiosurgery group of patients had been helpful.
"Results of this study show that initial stereotactic radiosurgery alone, coupled with close observation, could become the standard of care for patients newly diagnosed with brain metastases to best preserve their neurocognitive function," Chang said.
By Cynthia Keen
AuntMinnie.com staff writer
January 7, 2009
Related Reading
Stereotactic body radiotherapy aids patients with metastatic cancer, October 21, 2008
Stereotactic radiosurgery improves survival after melanoma brain metastases, May 24, 2007
Whole-brain radiation does not improve on stereotactic radiation, June 8, 2006
Long-term survival possible after radiosurgery for brain metastases, January 12, 2006
Stereotactic radiotherapy effective for pediatric brain tumors, October 23, 2003
Copyright © 2009 AuntMinnie.com