Although whole-body MRI using a short-tau inversion recovery (WB-STIR) sequence detects some bone contusions and fractures not found on initial radiographic bone surveys, the technique may not be ready to replace radiography in the initial assessment of traumatic injury in cases of suspected child abuse.
That finding is from a new study by researchers from Rhode Island Hospital and Brown University in Providence, RI. The study was led by Dr. Peter Evangelista, who presented the results at last month's annual meeting of the American Roentgen Ray Society (ARRS) in Boston.
Radiographic bone survey (RBS) has long been the accepted method of choice for evaluating nonaccidental trauma, particularly in children younger than 2 years of age. But the technique isn't foolproof.
"Its limitations are in the evaluation of acute nondisplaced rib fractures and nonosseous injury and fracture aging, which is imprecise at best," Evangelista said. "Some of these limitations are overcome by doing a follow-up radiographic bone survey in two weeks, which some have supplemented with bone scintigraphy."
WB-STIR capabilities
Whole-body STIR has been known to have high sensitivity in detecting edema and occult injury, and Evangelista said the assumption has been that the technique "would be very helpful with nonaccidental trauma."
The retrospective study reviewed 51 children (32 boys and 19 girls) who were referred for a brain MRI because of suspected abusive head injury. Their mean age was 6 months, ranging from 1 week to 37 months.
All children underwent both WB-STIR and a radiographic bone survey between June 2003 and November 2007. MR imaging was performed on a 1.5-tesla system (Magnetom Symphony, Siemens Healthcare, Malvern, PA). Acquisition time was approximately seven minutes per scan, with two or three procedures conducted per child, depending on the size of the child, and multiple surface coils used.
The RBS protocol included anterior, posterior, and lateral radiographs of a child's skull, as well as chest, abdomen, and spine images for a total of eight views, as well as two oblique radiographs of the ribs and a single radiograph of the extremities. Additional views were conducted as deemed necessary by a pediatric radiologist.
The mean interval time between RBS and WB-STIR was 2.4 days, ranging from zero to 13 days; 69% of the imaging scans were performed within two days.
Fracture identification
For fracture identification via WB-STIR, the researchers looked for direct signs, such as discrete hypotense fracture line, low-signal intensity reparative callus, and displacement of fracture fragments. Indirect signs with WB-STIR included bone marrow edema with and without paraosseous edema and subperiosteal edema.
Fracture aging was based on the initial RBS, with researchers defining an acute fracture as a cortical disruption or undulation with no periosteal reaction. For subacute fracture, researchers visualized periosteal reaction or fluffy callus with or without a discrete facture, while a chronic fracture showed signs of mature callus that was at least equal to cortical density.
The researchers identified 218 fractures based on an initial RBS and follow-up, and categorized them based on whether they were classic metaphyseal lesion (CML) injuries, also referred to as corner or bucket handle fractures through the metaphysis, which are considered be very specific for child abuse. Of the cases, 176 of the fractures were non-CML injuries, versus 42 CML injuries, which occurred in eight children. Whole-body STIR identified 147 (84%) of the 176 non-CML fractures. There were five acute anterior rib fractures missed by both RBS and WB-STIR.
Children's injuries
In the WB-STIR analysis, the researchers found 42 children (82%) with injuries that "were considered to be secondary to nonaccidental trauma," Evangelista said. "WB-STIR did not change the clinical decision of the cause of trauma in any case."
Whole-body STIR, however, detected "an additional 14 fractures that were not picked up on the initial RBS," Evangelista added. "They were all confirmed on follow-up radiographs. Nine of those [fractures] could be identified retrospectively, if you looked at the films."
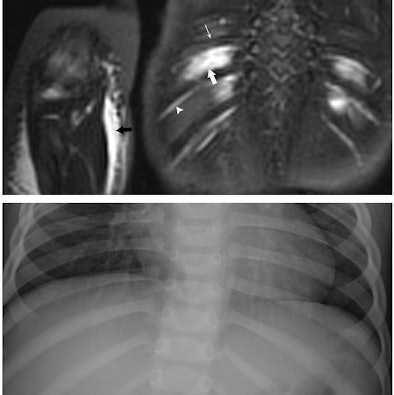 |
| Images are of a 17-month-old boy with suspected nonaccidental trauma. Coronal WB-STIR (top) of posterior chest wall and right elbow demonstrates edema of intercostal muscles (large arrow), but no fracture of adjacent ribs (thin arrow). Note normal hyperintense subcostal neurovascular bundle (arrowhead). There is diffuse subcutaneous edema of right antecubital fossa (black arrow) related to failed catheter placement. Corresponding RBS (bottom) corroborates absence of rib and elbow (not shown) fractures. Images courtesy of Dr. Peter Evangelista. |
Whole-body STIR also identified 43 additional soft-tissue lesions -- 34 (79%) were associated with fractures, five (12%) were iatrogenic (related to intramuscular injections), and four (9%) were deemed primary traumatic injuries. There were five additional hyperintense marrow foci that did not have any fractures on initial RBS or in follow-up, which were deemed to be traumatic bone edema.
False-negative results
The study also found an interesting disparity between WB-STIR and RBS in false-negative results among non-CML lesions. The initial RBS for acute fractures had a false-negative rate of 27%, compared with WB-STIR's false-negative rate of 8%. For chronic fractures, however, WB-STIR fared much worse, with a false-negative rate of 36%, compared with 0% for RBS.
But WB-STIR did add value in documenting additional injuries, he added. The technique detected 14 additional fractures among acute fractures that were later uncovered in RBS follow-up, as well as bone contusions and soft-tissue injuries.
The researchers concluded that WB-STIR may have a role in certain situations in the future, suggesting that a negative WB-STIR result and an initial RBS may allow the discharge of a child or limit follow-up RBS. However, MRI isn't ready to replace RBS for the initial examination of children with suspected trauma from child abuse.
"Whole-body STIR is not a standalone test, which is a little bit disappointing, and in no case did it change the clinical assessment as to the cause of the traumatic injury," Evangelista told ARRS attendees.
By Wayne Forrest
AuntMinnie.com staff writer
May 12, 2009
Related Reading
MRI helps find fractures among elderly female ED patients, April 29, 2009
MRI used to diagnose complex lung infections in children, October 16, 2008
MR parameters divulge depth of acute hamstring injuries, July 13, 2007
MRI keeps pace with rapidly evolving musculoskeletal systems of young athletes, May 20, 2007
Copyright © 2009 AuntMinnie.com