VIENNA - Radiological imaging together with the contribution of nuclear medicine is crucial in the diagnosis of inflammatory conditions. Inflammatory infectious conditions are endless in number and are basically diseases classified by the presence of micro-organisms in tissue. The process of inflammation is the body's reaction characterized by increased local blood flow, edema, pain, and recruitment of white blood cells in order to disinfect and remove the pathogen.
Inflammatory bowel disease (IBD) and vascular graft infection (VGI), which will be covered in this session in detail, are two conditions where both specialities, radiological imaging (RI) and nuclear medicine (NM), can contribute equally to finding the right diagnosis.
Inflammation, however, can also be seen in other degenerative diseases without the presence of pathogens. In these diseases, the inflammatory process is very similar to that of infections, but the recruitment of white blood cells is of a much lesser extent and mainly due to lymphocytes. Dr. Alberto Signore, from the department of nuclear medicine and molecular imaging at the University Medical Center, Groningen, points out the importance of an accurate differential diagnosis when dealing with inflammatory conditions.
"In most cases, we have to make a differential diagnosis between these two types of inflammation: a sterile inflammation versus a septic inflammation (infection) because prognosis is different and treatment is different. In the case of a sterile inflammation, it can be treated with anti-inflammatory drugs only and the prognosis is generally good. In the case of septic inflammation (infection), treatment is with antibiotics and/or surgery and the prognosis can be bad," said Signore.
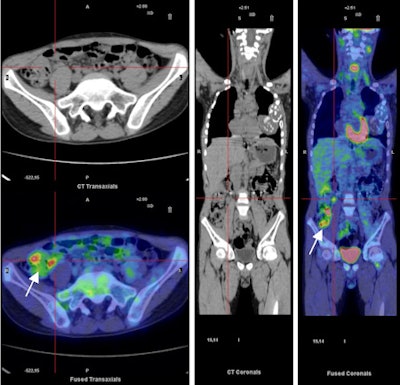 |
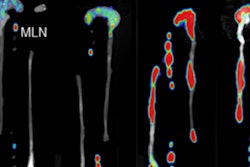
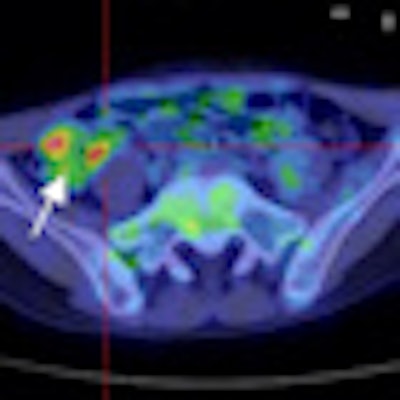
| F-18 FDG PET/CT images (trans-axial and coronal slides) in a patient with active Crohn's disease. Images show areas with increased glucose metabolism. A reactive lymphonode is detectable (defined by red lines) but it is not necessarily an infected site. The white arrow shows activity in the inflamed gut wall. Because of the lack of specificity of the radiopharmaceutical these areas can be inflamed or infected. A.W.J.M. Glaudemans, F. Maccioni, L. Mansi, R.A.J.O. Dierckx, A. Signore. Imaging of cell trafficking in Crohn's Disease. J. Cell. Physiol. 223: 562-571, 2010. |
Imaging modalities are crucial to making an accurate differential diagnosis between the two types of inflammation and also in evaluating the extent of the disease, as well as the progress and efficiency of treatment. In clinical practice, radiological modalities, including conventional radiology, ultrasonography, CT, and MRI, are the primary choice for assessing the site and extent of inflammation, for example the lungs, bowel, bones, joints, and brain. Edema and increased vascularity in inflammation can also be easily detected, but when it comes to differential diagnosis between sterile and septic inflammation, the specificity of radiological methods is not precise enough. Radiological imaging is very useful in evaluating the extent of inflammation and associated complications, but cannot be used to monitor the efficiency and progress of treatment in short intervals.
"The signs of inflammation that can be detected in RI are certainly less specific than in NM, whilst the radiological evaluation of the site and extent of the inflammatory process, however, is extremely accurate and more defined, particularly with CT and MRI, than with NM. Nuclear medical imaging, in general, has a lower spatial resolution and poorer anatomical detail, if we exclude hybrid imaging, like PET/CT and PET/MRI," explained Dr. Francesca Maccioni from the department of radiological sciences at "La Sapienza" University of Rome, Italy.
NM uses radiopharmaceuticals which, after intravenous injection, bind to the target in vivo and allow the desired target to be visualized. "To image infections we use radiopharmaceuticals against bacteria or, more often, granulocytes, which allow us to distinguish between sterile inflammations, which are poor in granulocytes, and septic inflammations, which are rich in granulocytes. The diagnostic accuracy of these techniques varies depending on the different body parts, but as it is always above 90% the clarification rate is higher than with conventional radiological techniques such as x-ray films, CT, or NMR," explains Dr. Signore.
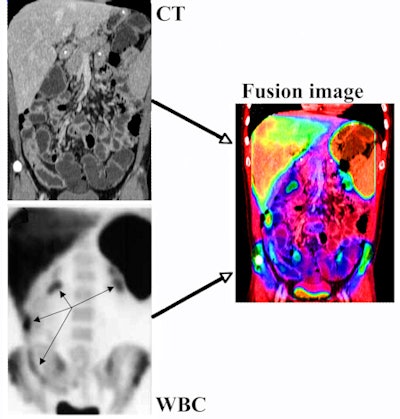 |
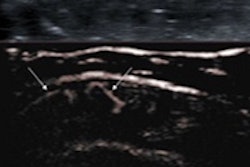
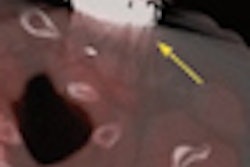
| CT enteroclysis (top left) shows a parietal thickening (10.8 mm) involving most ileum and particularly the distal part, with increased vascularity and a mesenteral hypertrophy. Technetium-99m-WBC scan (bottom left) shows only focal leukocyte infiltration in four different ileal segments (small arrows). The postprocessing fusion imaging of the two studies allows us to better co-localize the lesions and to obtain important pathophysiological information (parts of affected ileum are fibrostenotic without leukocyte infiltration; other segments show signs of acute inflammation). Similar information can be obtained using hybrid imaging with SPECT/CT. A.W.J.M. Glaudemans, F. Maccioni, L. Mansi, R.A.J.O. Dierckx, A. Signore. Imaging of cell trafficking in Crohn's Disease. J. Cell. Physiol. 223: 562-571, 2010. |
Unfortunately, nuclear medicine imaging methods are complex to perform and require specialized centers and equipment that precludes them from being a standard examination method for differential diagnosis of inflammation and also makes them quite expensive. In most cases the diagnostic protocol starts with radiological methods, partly due to their wide availability, and then if there is some doubt about the type of inflammation, it continues with a nuclear medicine examination.
Inflammatory bowel disease, which refers to both Crohn's disease (CD) and ulcerative colitis (UC), is a perfect example of how both methods can contribute to the patient's benefit. The main characteristic is a chronic, uncontrolled inflammation of the intestinal wall, which affects different segments of the small and large bowel in CD, and predominantly the colon in UC.
While high-resolution ultrasound (HRUS) combined with color Doppler or the use of CEUS allows detailed morphological evaluation of the affected bowel wall and assessment of the disease's activity, it strongly depends on the operator and lacks panoramic scope. On the other hand, the diagnostic capabilities of CT have improved since the introduction of multidetector technologies, although examinations still come with a significant radiation dose, which only allows for occasional clinical use. MRI combines the advantages of US and CT, as it involves no radiation exposure and provides high tissue contrast. MR enterography or enteroclysis have shown great accuracy in evaluating the morphological changes and complications of CD, while different imaging parameters, T1 and T2 weighted, allow bowel wall characterization and assessment of disease activity. Drawbacks in terms of technology dependence, low availability, and complexity of imaging parameters have to be accepted.
Nuclear medicine also offers several possibilities for the imaging of inflammatory bowel disease, with the use of radiolabeled autologous white cells (WBC) being the most discussed and common method. WBC allows the whole body to be evaluated with a single scan and can depict the extent of pathological gut wall infiltration by leucocytes, which are a sign of disease activity. Although there has always been criticism due to the long preparation time required and lack of anatomical accuracy, WBC methods have improved significantly through the introduction of new kits with technetium-99m and the option of using hybrid SPECT/CT cameras. A new indication for IBD has been found through the implementation of new SPECT and PET radiopharmaceuticals for molecular imaging and in vivo histological characterization of lesions, which makes the presence of activated T-cells or lymphokines (such as TNFa) in gut wall lesions measurable.
Asked for their preferred method for diagnosing and monitoring inflammatory conditions both experts gave surprisingly similar replies: "The combination of the two approaches provides different and more complete information to the clinician. When hybrid cameras (for RI and NM) are available, the patient can have both examinations at the same time. Integrated hybrid imaging is likely to be the future of both NM and RI. However, to obtain the most information, hybrid examinations should be evaluated jointly by a nuclear physician and a radiologist."
Hybrid cameras, which work through a combination of NM and MRI techniques, offer the clinician a deeper look at the molecular level of inflammatory diseases and make it easier to decide on individual therapeutic steps and to monitor the efficiency of treatments. Asked for his personal expectations regarding future imaging methods in inflammatory conditions, Prof. Signore, a nuclear medicine physician at "La Sapienza" University of Rome, Italy, and coordinator of the EANM task group on infection imaging, foresees a future affiliation between both methods: "Hybrid cameras are now available (PET/NMR, for simultaneous MRI and NM), the use of which will rapidly expand. I believe they constitute the future of the integrated imaging of inflammatory diseases together with the development of new ‘tailored' radiopharmaceuticals for diagnosis and therapy decision-making."
Overall, the session will focus on the integration of different imaging modalities and the gains that can be achieved by combining NM and radiological imaging methods. Talks about vascular graft infection from the radiological perspective as well as from the nuclear medicine perspective will be given by Dr. Alejandro Romero Jaramillo, from Vall d'Hebron University Hospital, Barcelona, Spain, and Prof. Ora Israel from Rambam University, Haifa, Israel, respectively.
Originally published in ECR Today March 1, 2012.
Copyright © 2012 European Society of Radiology