Delayed PET/CT with laxative-augmented contrast medium is more accurate than initial PET alone in the detection of colorectal cancer, according to a study published online March 15 in Radiology.
The researchers also concluded that this approach is promising for guiding decisions about how to treat patients with colorectal FDG foci. The lead author of the study is Dr. Yen-Kung Chen, PhD, from the nuclear medicine department and PET center at Shin Kong Wu Ho-Su Memorial Hospital in Taiwan.
As the researchers noted, colorectal cancers are associated with increased FDG uptake. "However, benign, infectious, inflammatory, and granulomatous processes also may cause an increase in FDG uptake," they wrote. "A focal and well-circumscribed intra-abdominal area of increased FDG uptake may be interpreted as equivocal or suggestive of malignancy without anatomic localization."
Past research has concluded that while PET/CT may be helpful for locating and characterizing foci of increased FDG uptake within the bowel, the interpretation of PET with CT characteristics resulted in false-positive rates of 13% to 29%, Chen and colleagues wrote.
Patient demographics
The researchers enrolled a total of 847 consecutive patients from November 2005 to December 2006 in the prospective study. The subjects, 471 men and 376 women, had a mean age of 50.7 years, ranging from 23 to 85 years. They all received FDG-PET or PET/CT scans as a part of their clinical care or screening program.
Among the 847 cases, 209 patients had a history of cancer and received FDG-PET or PET/CT as a part of their clinical care; 27 had newly diagnosed colorectal cancer and received FDG-PET or PET/CT for clinical staging.
The remaining 638 patients had no history of cancer and were part of a screening program. Among them, 152 underwent optional colonoscopy the day after their FDG-PET or PET/CT scans.
The study excluded patients who did not receive laxative-augmented contrast medium before delayed PET/CT or if they were lost to follow-up.
Imaging protocol
As part of the imaging protocol, patients received laxative-augmented contrast medium orally or by rectum; 500 mL of diluted 3% contrast medium (iothalamate meglumine, Conray 60, Covidien) was mixed with 125 mL of magnesium citrate (MagVac, Purzer Pharmaceutical).
Images were acquired on either a PET scanner (Ecat Exact HR+, Siemens Healthcare) or an integrated PET/CT scanner (Discovery LS, GE Healthcare).
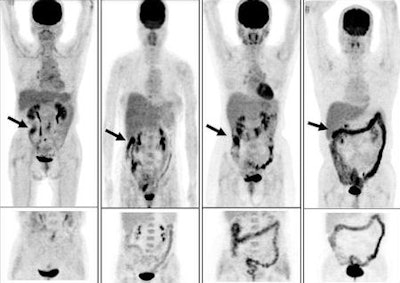 |
| Initial PET scans (top images) and PET scans obtained at delayed PET/CT after administration of oral laxative-augmented contrast medium (bottom images). The initial PET scans demonstrate colorectal FDG uptake patterns (arrow), as follows: (far left) nodular-focal pattern in ascending colon, (left) segmental pattern in hepatic flexure of colon, (right) nodular-multifocal pattern in colorectum, and (far right) diffuse pattern in transverse and descending colon. Images courtesy of Radiology. |
Images were read by two nuclear medicine physicians who were aware of the patients' clinical histories. However, the readers were not aware of results of other imaging examinations, if they were performed.
The analysis showed increased tracer uptake in the colon or rectum at initial PET examination in 138 (16%) of the 847 patients. The 138 patients underwent delayed PET/CT after administration of laxative-augmented contrast medium. Of the 709 patients who did not undergo delayed PET/CT after laxative-augmented contrast administration, 38 subjects were lost to follow-up.
In addition, one patient with increased colorectal tracer uptake was lost to follow-up. A total of 710 patients were excluded from further study, leaving researchers with a final study cohort of 137 patients.
FDG-PET results
Among those 137 patients, the uptake in abnormal FDG at initial PET was considered minimal in 14 (10%) of the 137 patients, equivocal in 68 (50%), and positive in 55 (40%). In the 14 patients with minimal uptake at initial PET, uptake was reclassified as positive in two patients and reconfirmed as minimal in 12 cases.
With laxative-augmented contrast medium and delayed PET/CT, the number of patients with equivocal findings decreased from 68 to 11 (84%). Among the 27 patients with newly diagnosed colorectal cancers, 24 were consistently classified as showing positive uptake at both initial PET and delayed PET/CT.
The remaining three patients with areas of equivocal uptake were reclassified as having positive uptake at delayed PET/CT.
"If we excluded 24 of the 27 known colorectal cancers from patients classified with positive uptake at initial PET and 27 known colorectal cancers revealing a positive grade at delayed PET/CT, the number of patients with positive findings decreased by 58.1% (from 31 to 13 patients)," Chen and colleagues wrote.
In addition, the researchers identified 24 true-positive findings, 74 true-negative findings, 31 false-positive findings, and eight false-negative findings with FDG-PET. With delayed PET/CT, there were 31 true-positive findings, 97 true-negative findings, nine false-positive findings, and no false-negative findings.
Image accuracy
The accuracy of initial PET was 72% (98 of 137 patients), while the accuracy of delayed PET/CT was 93% (128 of 137 patients).
The authors cited several limitations of the study, such as the use of only a single delayed scan with laxative-augmented contrast medium. Also, the study design did not account for the potential effect of a delayed scan obtained with and without laxative-augmented contrast medium.
In addition, because the location of the colorectal FDG focus cannot be determined before the initial scan, it is not possible to decide on the suitable laxative-augmented contrast medium protocol, the researchers wrote.
Based on the results, the researchers concluded that with a conventional PET or combined PET/CT imaging protocol, the use of a laxative-augmented contrast medium with delayed PET/CT "improved the diagnostic accuracy and reduced the number of equivocal and false-positive findings in patients with colorectal FDG foci."