FDG-PET shows "superior" ability to detect early-stage neuroblastoma, whereas scintigraphy with iodine-123 metaiodobenzylguanidine (I-123 MIBG) can be beneficial in detecting the pediatric disease in more progressed stages, according to a study published in the August issue of the Journal of Nuclear Medicine.
Researchers at Cincinnati Children's Hospital Medical Center in Ohio and St. Jude Children's Research Hospital in Memphis, TN, also noted that FDG-PET provides important information at major decision points during therapy, such as stem cell transplantation or before surgery (JNM, August 2009, Vol. 50:8, pp. 1237-1243).
Neuroblastoma's prevalence
Neuroblastoma accounts for 6% to 10% of all childhood cancers in the U.S. and 15% of cancer deaths in children. Identifying the location and progression of the disease is critical for managing its treatment, which can include surgery, chemotherapy, radiation, bone marrow transplant, or investigational therapies. Some 650 new cases of the cancer are reported in the U.S. each year, according to the National Cancer Institute (NCI).
The researchers retrospectively reviewed pairs of 113 I-123 MIBG and FDG-PET scans in 60 patients from both hospitals, according to lead author Dr. Susan Sharp from Cincinnati Children's Hospital and colleagues. The 23 girls and 37 boys had a median age at diagnosis of 3.1 years and confirmed cases of neuroblastoma. The paired scans were acquired within 14 days of each other, between January 2003 and October 2007.
FDG-PET scans were acquired after administration of 5.18 or 5.55 MBq/kg dose of fluorine-18 FDG, with a maximum dosage of 444 MBq. A total of 85 FDG-PET scans were performed at St. Jude's (Discovery LS, GE Healthcare, Chalfont St. Giles, U.K.), and 27 FDG-PET scans were conducted at Cincinnati Children's (12 scans on Exact or Accel PET, Siemens Healthcare, Malvern, PA, and 15 scans on a Discovery STE PET/CT scanner, GE).
All MIBG scans were acquired using I-123 MIBG with administration of either 5.18 MBq/kg or 370 MBq/kg, with a maximum dose of 370 MBq. A total of 110 I-123 MIBG scans included 24-hour, whole-body, and SPECT images.
Early detection
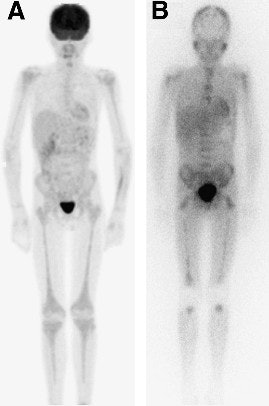
In patients with stage I and II neuroblastoma, FDG-PET found more primary tumor or local or regional metastases than I-123 MIBG scintigraphy in nine of 13 scans (69%) with a 95% confidence interval in six patients.
FDG-PET and I-123 MIBG were equivalent in one of 13 scans (8%) with a 95% confidence interval in one patient imaged at diagnosis. Findings were negative in three of thirteen FDG-PET and I-123 MIBG scans (23%) with a 95% confidence interval in three patients imaged after tumor resection.
For patients with stage III disease, I-123 MIBG depicted more extensive primary tumor or local or regional metastases in five of 15 scans (33%) with a 95% confidence interval in four patients. The scans included three FDG-PET scans with negative results in three patients with I-123 MIBG-positive neuroblastoma imaged during initial chemotherapy or before stem cell transplantation. FDG-PET depicted more extensive primary tumor or local or regional metastases in four of 15 scans (27%) with a 95% confidence interval in four patients.
In stage IV neuroblastoma cases, I-123 MIBG proved more helpful, discovering more neuroblastoma sites in 44 of 85 scans (52%) with a 95% confidence interval in 24 patients. FDG-PET found more neuroblastoma sites in 11 of 85 scans (13%) with a 95% confidence interval in eight patients.
 |
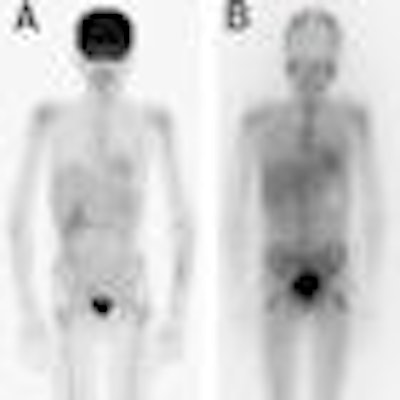
| Image of a 13-year-old male with stage IV neuroblastoma after initial chemotherapy shows FDG-PET (A) demonstrating mild diffuse bone marrow uptake extending throughout axial and appendicular skeleton in response to marrow expansion. I-123 MIBG (B) illustrates uptake in diffuse bone or marrow metastases. Researchers noted the absence of I-123 MIBG uptake in mid- or distal humerus and mid- or distal tibia. Images courtesy of the Journal of Nuclear Medicine, Cincinnati Children's Hospital Medical Center, and St. Jude Children's Research Hospital. |
In the stage IV disease follow-up, more than 12 months after the beginning of therapy, there were 34 scans (20 patients). I-123 MIBG depicted more neuroblastoma sites in 17 scans of 10 patients. According to the authors, the detections were "primarily because of depiction of bone or marrow metastases, but also because of the depiction of some local or regional metastases, including five FDG-PET scans with negative findings in three patients with I-123 MIBG-positive neuroblastoma."
The analysis also found that FDG-PET depicted more metastatic disease in three scans in three patients, while I-213 MIBG and FDG-PET were equivalent in three scans in three patients.
'Superior' FDG-PET
With those results, the researchers concluded that FDG-PET is "superior in depicting stage I and II neuroblastoma, although I-123 MIBG may be needed to exclude higher-stage disease." FDG also provides important information in patients with tumors that weakly accumulate I-123 MIBG and at major decision points during therapy (i.e., before stem cell transplantation or surgery).
In addition, the researchers determined that FDG-PET also performed better when delineating the progression of the disease in the chest, abdomen, and pelvis and "should always be considered when I-123 MIBG reveals less disease than suggested by clinical symptoms or conventional imaging modalities."
The researchers did caution, however, that the use of I-123 MIBG scintigraphy and FDG-PET in neuroblastoma will have "frequent exceptions that could significantly affect clinical management of individual patients. Larger multi-institutional, prospective trials may be necessary to provide further information."
By Wayne Forrest
AuntMinnie.com staff writer
August 3, 2009
Related Reading
Study: Childhood cancer rates remain constant, May 28, 2009
SPR group tackles radiation dose in pediatric nuclear medicine, May 22, 2009
Passport for Care aids follow-up of childhood cancer survivors, April 13, 2009
Childhood cancer survivors have increased risk of developing new malignancies, December 31, 2007
Tips for successful pediatric nuclear imaging, October 20, 2006
Copyright © 2009 AuntMinnie.com