PET demonstrates excellent diagnostic capabilities in detecting coronary artery disease, and is superior to perfusion imaging, CT angiography (CTA), and MR angiography (MRA), according to a retrospective review of PET research studies over a 30-year period.
With past studies noting PET's high sensitivity and specificity, the researchers of the current study recommend the modality be used more often as an initial test to diagnose coronary artery disease.
The group from the University of Michigan Health System in Ann Arbor reviewed studies from January 1977 to July 2007 using Medline and Embase, and published its findings in Academic Radiology (April 2008, Vol. 15:4, pp. 444-451). The analysis included cases in which PET was used as a diagnostic test for coronary artery disease and catheter x-ray angiography was used as the reference standard. The data were reviewed at the patient level, with secondary analyses conducted at the coronary territory level.
'High specificity'
According to the results, PET appears superior to perfusion imaging with thallous chloride Tl-201 and sestamibi, and anatomical imaging using multidetector CTA or MRA.
"What we found after looking at 19 studies and more than 1,400 patients is that PET's high specificity and sensitivity are better than almost all forms of functional imaging and likely all anatomical imaging," said study co-author Dr. Kiran Nandalur, a staff radiologist at William Beaumont Hospital in Royal Oak, MI.
On the patient level, PET demonstrated a sensitivity of 92% and specificity of 85% in detecting luminal stenoses. On the coronary territory level, PET showed a sensitivity of 81% and specificity of 87%. The prevalence of coronary artery disease in the group of 1,442 patients was 77%.
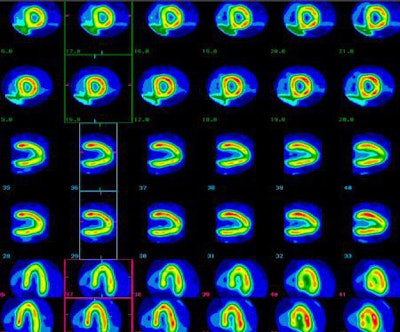 |
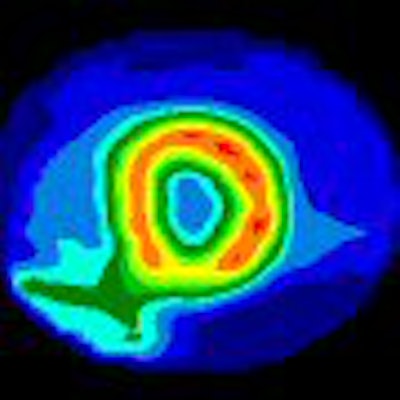
| Clinical images show a 65-year-old male with preoperative stress PET perfusion MRI with NH3 demonstrating short-axis and horizontal and vertical long-axis views, with stress (superior) and rest (inferior) images. Images demonstrate reversible defects involving septal and lateral walls, and corresponding obstructive coronary plaques were found in the left anterior descending artery and left circumflex artery on coronary angiography. Image courtesy of Drs. Paresh Mahajan and Darlene Fink-Bennett of William Beaumont Hospital. |
Based on the review of previous studies, PET has shown to be "cost-effective in the workup of (coronary artery disease) relative to exercise testing, SPECT, and immediate angiography," the researchers noted. "Moreover, myocardial perfusion imaging with PET has significant prognostic value for predicting cardiac events, such as death and myocardial infarction, including patients whose diagnosis is less certain after SPECT and obese patients."
Limiting factors
As for why PET has not been utilized more extensively in nuclear cardiology, the researchers stated that it could be due to cost, the availability of the modality, or healthcare providers being unaware of its performance.
The group was surprised to find that three studies showed PET/CT with lower specificity than PET alone, despite CT's addition of anatomical information to the image, according to Nandalur.
"It is surprising, because the PET/CT studies were done within the last three years and they are of much higher quality," he said. "The PET studies were done in the 1990s and late 1980s and were lower-quality studies. You'd expect the PET/CT results to be more accurate, so it is surprising to say that PET/CT is less accurate than PET."
PET with CTA
Nandalur plans to follow this study with additional research to better determine PET/CT's capabilities for coronary artery disease detection. He sees PET's functional imaging and CTA angiography's anatomical imaging as the potential gold standard for this application.
One drawback of CTA alone is that the contrast agent can overestimate the degree of luminal stenosis in an artery by brightening calcium deposits.
"PET will work no matter what, because it sees the perfusion in the myocardium," Nandalur said. "Coronary CT lets you look at the coronary artery for obstructed lesions. Sometimes, if you have a calcified lesion, it overestimates the degree of luminal stenosis. That's why if you can combine the information from PET and CT angiography, it would be very helpful in determining if something is real or not."
If PET reveals an abnormality and the CT angiogram appears normal, a clinician may find that a calcified lesion is causing a real stenosis rather than a false positive, according to Nandalur. "Conversely, if you have a stenosis and you can clearly see the stenosis on CTA, but it is negative on PET, maybe it isn't causing that much hemodynamic effect and maybe it doesn't need to be corrected," he said.
By Wayne Forrest
AuntMinnie.com staff writer
March 28, 2008
Related Reading
Israeli group test-drives 64-slice SPECT/CT system for cardiac imaging, June 6, 2007
Automated emission correction shows potential for cardiac PET/CT, March 9, 2007
PET identifies inflammation severity in carotid plaques, November 21, 2006
PET perfusion can predict cardiac events, March 15, 2006
PET, SPECT measures of LVEF have superior predictive value, March 13, 2006
Copyright © 2008 AuntMinnie.com




















