MRI has a "distinct advantage" over standard radiography in detecting hip or pelvic fractures among elderly patients brought to an emergency room for care, according to a study published in the April issue of the American Journal of Roentgenology.
Researchers at Duke University Medical Center in Durham, NC, found that the newly detected fractures can help steer patients to the appropriate medical and surgical therapy and, thus, possibly avoid hip replacement. The lead author of the study is Dr. Matthew Kirby (AJR, April 2010, Vol. 194:4, pp. 1054-1060).
"In our ER practice, if we don't see an obvious fracture and there is a concern, our knee-jerk response is to get an MRI to see if there is a fracture we are missing," said study co-author Dr. Charles Spritzer, professor of radiology at Duke. "We had a patient group that we were recommending for MRI routinely. What wasn't clear to us was whether it was a good recommendation, and how often it changed what was going on."
The researchers reviewed Duke's MRI database for lower-extremity MRI exams from July 2005 through June 2008, looking for patients who had undergone x-ray of the hip, pelvis, or femur in the emergency department and received a diagnostic MRI scan of the hip or pelvis within one calendar day.
Elderly patients
The average age among the 92 patients in the study group was 70.8 years, with a range of 19 to 94 years. There were 77 women and 15 men. All patients received at least one x-ray exam of the hip, pelvis, or femur; 71 patients underwent at least two x-ray studies.
MRI exams were conducted on either a 1.5-tesla system (Magnetom Symphony and Magnetom Avanto, Siemens Healthcare, Malvern, PA; or Signa HDx 1.5T, GE Healthcare, Chalfont St. Giles, U.K.) or 3-tesla system (Magnetom Trio, Siemens; or Signa HDx 3T, GE). All examinations were performed with a phased-array torso coil.
Two musculoskeletal radiologists interpreted the MR images for fractures, bursitis, tendinopathy, muscle injury, and other potential causes of pain.
There were 97 MRI scans among the 92-patient sample. Five patients received bilateral examinations, 56 exams were of the right hip, and 41 scans were of the left hip. Sixty-five of the 92 patients had a documented history of trauma: The most common incident among elderly patients was a fall, whereas a motor vehicle collision was most common among patients younger than 50.
In the retrospective review, MRI detected 63 fractures in 33 patients, and x-rays were positive or suggestive of a fracture of the hip or pelvis in 26 patients. MRI discovered no signs of fracture in 11 of the 92 patients (12%).
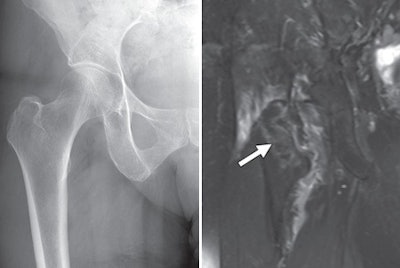 |
| Images are of an 80-year-old female patient with osteopenia and radiographically occult intertrochanteric fracture of the right hip. The anteroposterior x-ray image (left) does not show a fracture, while the coronal fat-suppressed T2-weighted MR image (right) shows marrow edema consistent with nondisplaced fracture (arrow). Images courtesy of the American Journal of Roentgenology. |
MRI discoveries
Most important, MRI discovered 23 fractures of the hip or pelvis among 13 patients (14%) with normal x-ray findings. In another 15 patients who had abnormal x-ray findings, MRI detected 12 additional pelvic fractures not identified on the x-rays.
According to Spritzer, the most surprising result was that 26 fractures were called or queried on x-ray. "These were not definite displaced fractures, but they were ones we were comfortable with," he said. "Only 11 of those fractures were wrong. If we didn't use MRI, we would have sent 11 patients to be pinned unnecessarily."
While "any unnecessary examination is to be regretted, because of the high morbidity and mortality of hip and pelvic fractures," the authors wrote, "a generous false-positive rate for radiography and subsequent MRI follow-up is not unreasonable in this patient population."
Hip replacement
The discovery of a hip or pelvic fracture, especially in an elderly patient, is important because prompt, proper treatment may help avoid hip replacement. "If the hip is replaced, some studies show one-year mortality can approach 40%," Spritzer said.
He added that it's unclear whether the hip fracture causes a patient's health to deteriorate or if the hip fracture is a sign that an older patient is in poor health already, "but anecdotally I have seen patients who are doing fine, then they break their hip, and they spiral down."
From a treatment point of view, Spritzer said the preference is to intervene and save a patient's hip without having to replace it. "That's why it is important not to miss [fractures] in this patient population," he said.
The accurate diagnosis of hip and pelvic fractures in the emergency department also can help reduce the rate of hospital admissions among patients who do not have fractures.
The study results have not prompted any change in Duke's ER practices, however, and x-ray remains the first course of action to detect hip and pelvic fractures.
'MRI is appropriate'
"There are cases where it is clearly a fracture, there is no doubt, and it is clear what needs to be done," he said. "If you have an osteopedic person who has fallen, the clinical history and clinical exam are concerning for fracture, and plain film definitely does not show [a fracture], I think MR is appropriate and should be the next step."
The authors noted several study limitations. Because the study evaluated only patients who underwent MRI scans, workup bias may have been present in the sample. "We attempted to mitigate this bias by evaluating all pelvic MRI examinations performed and including examinations of all adults with suspected fractures regardless of trauma history, comorbid conditions, and age," they wrote.
"Second, although most of our sample had a history of trauma, we did not attempt a separate analysis of the trauma patients," they continued. "This choice was made partly because of the incomplete and sometimes incorrect history available at emergency department admission, a history often complicated by dementia or unwitnessed events."
By Wayne Forrest
AuntMinnie.com staff writer
April 7, 2010
Related Reading
MRI finds hip, pelvic abnormalities in healthy hockey players, March 23, 2010
3T MRI as good as MR arthrography for planning hip surgery, February 1, 2010
Isotropic 3T MRI aids in diagnosing labrum, rotator cuff tears, December 29, 2008
MRI keeps pace with rapidly evolving musculoskeletal systems of young athletes, May 20, 2007
The ABCs of MRI for hip disorders, February 2, 2007
Copyright © 2010 AuntMinnie.com