SAN FRANCISCO - Colorectal cancer screening compliance doubles when primary care physicians do their own patients' colonoscopies -- under expert supervision. What's more, exam quality is "outstanding," said an internal medicine physician describing what he called a "radical" colorectal cancer screening solution.
In a Saturday presentation at the American Society of Clinical Oncology (ASCO) Gastrointestinal Cancers Symposium, Stephen Lloyd, MD, PhD, said his pilot program to boost colonoscopy screening in a population of more than 30,000 patients in Columbia, SC, has delivered the highest compliance rate, the highest adenoma detection rate, and the lowest complication rate ever reported.
A radical solution?
Colorectal cancer (CRC) screening needs a radical solution because compliance rates aren't rising significantly, but cancer cases are, Lloyd said in his talk. More than 150,000 CRC cases and 50,000 deaths per year in the U.S. make colorectal cancer the single major cause of death for nonsmokers in the U.S. -- and the toll is rising. In 2011 the American Cancer Society predicts that colorectal cancer deaths will increase by some 9% -- or an additional 4,400 patients, Lloyd said.
"We're losing the battle. Why? I'm not sure why any patient would be reluctant to go see a doctor who wants to cram a five-foot hose up their derriere," Lloyd quipped.
Not all patients will accept invasive colonoscopy, Lloyd told AuntMinnie.com. That makes virtual colonoscopy an essential component in any campaign to increase compliance.
But what makes most patients willing to endure colonoscopy screening is having their own primary care physician, whom the patients know and trust, operating the colonoscope, Lloyd said. The new model is starkly different from current practice patterns, in which the primary care physician refers patients to a gastroenterologist. On average, only 50% of these patients show up for screening, Lloyd said.
A new paradigm
Lloyd said he and his colleagues will soon publish the results of their experience with the South Carolina pilot screening program in which "these primary care doctors have a higher than 80% compliance rate in age-appropriate individuals," he said. "From a capacity standpoint in Columbia, 30% of the primary care physicians are now involved in performing their own colonoscopies."
If half of that percentage -- 15% of U.S. primary care physicians -- switched to the new model, it would achieve the "magic number" of 6 million patients who need to be screened each year to keep up with America's aging population. Half of these physicians have already been performing flexible sigmoidoscopy.
How can primary care docs perform colonoscopies -- a small percentage of which are difficult to complete due to the twists and turns of the colon, or result in the detection of more challenging findings such as large polyps or flat polyps? By having an experienced gastroenterologist onsite to take over difficult cases, Lloyd said.
"We have a model where there's an expert always present to be able to 'rescue' primary care physicians," he said. As a result, primary care physicians are never out of their comfort zone. The physicians "can be confident when they invite their patients for screening that they are going to get an excellent and safe test."
The South Carolina colon screening center has approximately 30 primary care physicians under the watchful eye of the gastroenterologist, Lloyd said. For each physician's first 150 cases, the gastroenterologist supervises each procedure sitting in the same room as the primary care physician. Thereafter, the gastroenterologist is in the next room training another primary care physician, while the previously trained physician works with the technologist in an adjacent room.
The primary docs use a "double-fisted" maneuver to insert the colonoscope -- i.e., two-handed -- while a technologist controls the rate of insertion and withdrawal and operates the control pad (up, down, right, left, air, water, and suction). In the 10% to 15% of cases where the colon is difficult to maneuver, or findings are more difficult to treat, such as with flat polyps or large polyps, the gastroenterologist is called to "rescue" the case and safely complete the endoscopy. The results have been extraordinarily positive, Lloyd said.
In the typical care model, it is the gastroenterologist who operates the colonoscope with his dominant hand while controlling it with the left. "It's cumbersome," Lloyd said. To date, 30,000 screening colonoscopies have been done in the program, with a very high adenoma detection rate and low complication rate, Lloyd said. More than 10,000 patients were included in a recently published analysis of a subset of these patients.
The analysis found a cecal intubation rate of 98.1%. Polyps were detected in 63.1% of patients, including a hyperplastic polyp in 27.5%, adenoma in 29.9%, advanced neoplasia in 5.7%, and cancer in 0.63%, with major adverse events in 0.06% (including two perforations and no deaths) (Xirasagar et al, Medical Care, August 2010, Vol. 48:8, pp. 703-709).
"Systems that use [primary care physicians] with specialist backup support enable high-quality colonoscopy performance," the authors concluded.
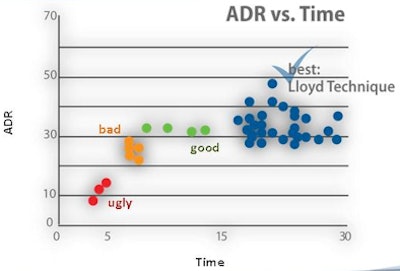
The big question, according to Lloyd, is "if we get them to improve compliance and address capacity, what's going to happen to the quality?" The answer is that it has soared, he said. In 30,000 cases, the average adenoma detection rate (ADR) was 34% of patients, compared to a U.S. national average of 20%.
Typical adenoma detection rates are low and extremely variable in the U.S., Lloyd said. To illustrate, a 2006 study by Barclay and colleagues found large differences in the adenoma detection rate among 12 trained, board-certified gastroenterologists, which correlated closely to the time spent withdrawing the colonoscope, Lloyd said. The more time spent, the higher the adenoma detection rate (New England Journal of Medicine, December 14, 2006, Vol. 355, pp. 2533-2541).
Surprisingly, Lloyd said, the difference between the best- and worst-performing gastroenterologists was more than 1,000%. More to the point with regard to the present study, even the best group that spent the most time withdrawing the colonoscope had an adenoma detection rate of 30%, far greater than the U.S. average but less than what Lloyd's model is achieving.
Unfortunately, even five years after the Barclay study was published, organized gastroenterology has done little to address the problem of low adenoma detection rates. What's needed is an organization not affiliated with gastroenterologists to compel minimum performance standards for gastroenterologists performing colonoscopy and publish them, Lloyd said. Outside of the proposed model, there is tremendous variability in adenoma detection rates and quality control that is not being adequately addressed within the gastroenterology community.
New results
For the results Lloyd presented in his ASCO talk -- to be published this coming spring, he said -- 30 primary care physicians were recruited in Florida and South Carolina. Compliance rates within practices were measured before and after enrollment, and the quality metrics of the colonoscopies performed were evaluated.
"These 30 doctors have each performed above the experience of our best and brightest gastroenterologists," Lloyd said.
According to the results, compliance more than doubled -- from 38% to 84% -- when the primary care physician performed the colonoscopy, Lloyd reported. The gross completion rate (the rate at which the colonoscope reached the cecum) was 98.3%. The adenoma detection rate was 34%. Complications were the lowest ever reported.
 |
| In a cohort of 30,000 patients, mean adenoma detection rate (ADR) was 34% of patients using the supervised primary care physician model (blue dots). In comparison, green, yellow and red dots show three tiers of lower adenoma detection rates from 12-board certified gastroenterologists in a 2006 analysis of colonoscopy performance. The U.S. national average ADR is 20% of Image courtesy of Stephen Lloyd, MD, PhD. |
"We've augmented the capacity so that we can get to where we can screen 80% of the population and the quality is outstanding," Lloyd said. "Our adenoma detection rate is 34% and the national average is 20%."
"We had one perforation per 5,000 patients -- out of 30,000 patients, we've had three admitted to the hospital for bleeds," he said. Typical perforation rates for colonoscopy are approximately one of 2,000 patients, or one of 1,000 patients when polypectomy is performed.
If replicated nationally, the method has the potential to save more than 25,000 lives a year. Participation of the patient's primary care provider is a "powerful influence for improved compliance," Lloyd said. The availability of an expert to monitor results and "rescue" difficult cases results in outstanding results and safety for colonoscopy, he said.
But not all gastroenterologists are on board with the program -- in fact some in South Carolina have sued several times to stop the practice, Lloyd told AuntMinnie.com. "This campaign has been confronted with tenacious opposition from the gastroenterology community," he said.
In an interview with AuntMinnie.com after the talk, gastroenterology expert David Lieberman, MD, from Oregon Health Sciences University in Portland expressed concern that primary care physicians are few in number and very busy, with potentially little time to learn how to perform colonoscopy. Lloyd responded that the commitment is only two hours per week after training -- and half of these physicians are already practicing flexible sigmoidoscopy.
With the days of polio long past, what the U.S. needs is a new campaign modeled on that of vaccine pioneer Jonas Salk, MD, who wiped out polio a half-century ago. The new campaign will be known as SALC for "Saving American Lives with Colonoscopy," Lloyd said.
"I believe we can virtually eliminate suffering from CRC just like we did with polio in 1954," he said. "But it's not going to be easy."
By Eric Barnes
AuntMinnie.com staff writer
January 25, 2011
Related Reading
Study confirms accuracy of VC for bone mineral density exams, January 20, 2011
In partnership, some gastroenterologists embrace VC, November 15, 2010
VC may increase colon cancer screening, survey shows, November 10, 2010
VC advocates tout aggressive strategy for screening coverage, October 26, 2010
Higher colonoscopy complication rates found in seniors, October 19, 2010
Copyright © 2011 AuntMinnie.com