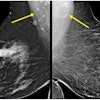
Annual breast cancer screening starting at age 40 yields the most mortality reduction, according to research published February 20 in Radiology.
A team led by Debra Monticciolo, MD, from Dartmouth in New Hampshire found that starting annual screening at this age and continuing to at least age 79 leads to the highest reduction in mortality with minimal risks.
“We’re hoping that not just radiologists, but primary care physicians will see this and realize the benefits of annual screening and how minimal the risks really are of this life-saving technique,” Monticciolo told AuntMinnie.com.
Debate continues on when and how often women should undergo breast cancer screening. Professional societies such as the American College of Radiology (ACR) and the Society of Breast Imaging (SBI), among other organizations, advocate for annual screening starting at 40. The U.S. Preventive Services Task Force (USPSTF), meanwhile, recommends biennial screening starting at this age, a B-grade recommendation.
Monticciolo and colleagues analyzed the Cancer Intervention and Surveillance Modeling Network (CISNET) 2023 median estimates of breast cancer screening outcomes. This data allows researchers to estimate screening outcomes at various frequencies and starting ages using U.S. data.
The researchers compared screening benefits in four different scenarios: biennial screening of women ages 50-74 (the previous USPSTF recommendation), biennial screening of women from 40-74, annual screening from 40-74, and annual screening from 40-79. CISNET does not offer modeling past age 79. They also took into account mortality reduction, life years gained, breast cancer deaths avoided, and risks that included benign, or unnecessary, biopsies, and recall rates.
The team reported that annual screening of women ages 40-79 with either digital mammography or tomosynthesis showed a mortality reduction of 41.7%. Biennial screening of women 50-74 and 40-74 achieved mortality reductions of 25.4% and 30%, respectively.
Annual screening of women 40-79 years also demonstrated the lowest per mammogram false-positive screens (6.5%) and benign biopsies (0.88%) compared with other screening scenarios, the researchers found.
Finally, the team found that women have a less-than-1% chance of having a benign biopsy following annual screening. Meanwhile, recall rates for annual screening mammography were under 10% while annual tomosynthesis led to a recall rate of 6.5%.
Monticciolo said she and her colleagues hope these results will add further support for annual screening starting at age 40.
“It’s the best way to get the most benefit and the most mortality reduction,” she told AuntMinnie.com. “And it really has the lowest risk on a per-exam basis.”
In an accompanying editorial, Bonnie Joe, MD, PhD, from the University of California, San Francisco, wrote that breast imagers are “well positioned to contribute to the science of screening and to promote early detection of breast cancer.”
While research on tracking initial methods of detection is being performed, she added that it “seems safest” to follow the ACR’s recommendations for every woman to undergo breast cancer risk assessment by age 30 and, if of average risk, start annual screening at age 40 and continue past 75 unless severe comorbidities limit life expectancy.
The full study can be found here.