Ultrasound-guided microwave ablation (MWA) is a safe, effective method for treating bone metastases, according to research presented May 9 at the American Roentgen Ray Society (ARRS) annual meeting.
In his talk, Zirui Zhang from the Sichuan Clinical Research Center for Cancer in China reported a perfect technical success rate with little to no complications in patients with this technique.
“Ultrasound-guided percutaneous MWA can provide short- to medium-term pain relief and functional improvement for patients with bone metastases, which is helpful to improve patients’ quality of life,” Jiang said.
Previous reports indicate that between 30% and 70% of patients with malignant tumors will eventually develop bone metastases. Of the symptoms, pain is the one most observed in patients and is persistent. Current treatment methods include medication, targeted therapy, radiotherapy, and surgery. However, each has its share of tradeoffs.
Thermal ablation has demonstrated its utility as a curative method for benign lesions and a palliative care method for metastatic tumors in the lungs, liver, and breast, among other areas. Jiang however noted that such data on bone metastases is limited.
As a result, the researchers sought to explore the clinical efficiency of ultrasound-guided percutaneous MWA in patients with painful bone metastases. The prospective study included 15 patients with 25 total bone metastases, all of whom underwent MWA.
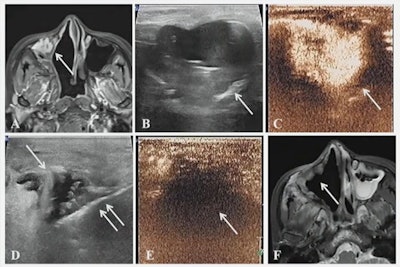 A case presented at the ARRS annual meeting shows the results of successful microwave ablation (MWA) treatment for a 39-year-old female with metastatic fibrosarcoma of the right axillary sinus.
A case presented at the ARRS annual meeting shows the results of successful microwave ablation (MWA) treatment for a 39-year-old female with metastatic fibrosarcoma of the right axillary sinus.
Metastases were located on the ribs, skull, pelvis, spinal cone, and sternum. Pathological types included sarcomas (32%), adenocarcinomas (32%), squamous carcinomas (24%), and types labeled as “other” (12%).
MWA had a technical success rate of 100%, with no severe complications being reported among the patients.
It also led to pain scores -- as defined by the 0-to-10-point numerical rating scale -- that significantly decreased from pre- to post-operation. Additionally, MWA led to significant increases in the Musculoskeletal Tumor Society (MSTS) scoring system. This scoring system ranges from zero to 30, with lower scores meaning high disability and higher scores indicating no impairment.
Jiang also presented some case reports, including one case that described where a 39-year-old was treated for metastatic fibrosarcoma of the right maxillary sinus. Images taken 12 months after MWA showed that the tumor had disappeared.
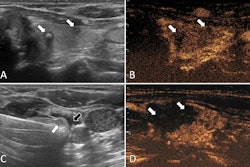
In another case, MWA was used for post-operative rib metastasis of a gastric stromal tumor. Ultrasound images acquired after MWA showed no enhancement and the patient reported no pain.
Jiang said that future studies with more patients and longer follow-up periods are needed to confirm the team’s findings.